A bad trip, also known as an acute adverse reaction to hallucinogenic drugs, can include a range of symptoms, such as anxiety, paranoia, delusions, hallucinations, and disordered thinking. These symptoms can be distressing and can potentially lead to dangerous behavior or harm to oneself or others. And even outside of negative scenarios, Bad Trip can be a challenging experience for the individual who is undergoing it. Therefore, it is better to be ready and know about First Aid for Bad Trip
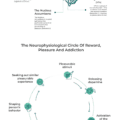
The exact mechanisms of these adverse reactions are not fully understood, but it is believed to be related to the way that hallucinogens interact with the brain. Hallucinogenic drugs can activate serotonin receptors in the brain, which can lead to changes in perception, mood, and thought processes. It is thought that these changes in brain function can trigger the onset of acute adverse reactions.
Treatment and First Aid for Bad Trip can involve several approaches, including:
- Reassurance and supportive care: Providing reassurance and supportive care can help to calm the person and prevent further escalation of symptoms. Encourage the person to focus on their breathing and help them to feel safe and supported.
- Benzodiazepines: Benzodiazepines are a type of medication that can help to reduce anxiety and agitation. They can be prescribed by a healthcare professional and should only be used under medical supervision.
- Antipsychotic medications: In cases where the person is experiencing severe hallucinations or delusions, antipsychotic medications may be prescribed by a healthcare professional.
- Management of physical symptoms: In some cases, hallucinogenic drugs can cause physical symptoms such as nausea or vomiting. Treatment may involve managing these symptoms with medications or other interventions.
We will focus on the first type of help for a Bad Trip (Reassurance and supportive care), because it is available to everyone, does not require special knowledge, is not associated with taking strong psychoactive drugs and can really extinguish the nightmare unfolding in a person’s consciousness and perception. This approach is ideal as first aid for bad psychedelic trip.
But first we need to learn to recognize when it’s time to intervene and the person most likely needs help.
Bad Trip or Psychotic Disorder?

Recognizing when a person is having a bad trip is essential for providing timely support and assistance.
What is interesting here is that medical diagnostic manuals do not have a separate field for the condition of a Bad Trip (as I know). Instead, there is a more severe and, if I may say so, pathological condition as Substance-Induced Psychotic Disorder (SIPD).
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) lists the following diagnostic criteria for SIPD:
- The presence of one or more psychotic symptoms (e.g. delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior)
- Symptoms developed during or soon after substance intoxication or withdrawal
- Symptoms are not better explained by a primary psychotic disorder (e.g. schizophrenia)
- Symptoms are not due to a medical condition or medication side effect
As we can see, this is a fairly general category, where, if desired, a Bad Trip can always be defined. But in practice, a Bad Trip will not always be SIPD. I would characterize a Bad Trip as a prodromal and abortive phas-type of SIPD.
Recognize when a Bad Trip is happening

The most important thing here is that a Bad Trip can be more controllable and reversible on average than a full-fledged Psychotic Disorder. And with competent actions, a person can “stay on the edge” without falling into a state for which hospitalization is most likely required. It is also important to distinguish a Bad Trip from other urgent conditions, for example, First Aid Serotonin Syndrome. And for all this, we must be able to recognize al teast common signs of a Bad Trip. Here they are:
Intense fear or anxiety: A person experiencing a bad trip may express extreme fear or anxiety and may feel like they are losing control.
Confusion or disorientation: The person may become disoriented, confused, or have difficulty understanding their surroundings.
Hallucinations: The person may see, hear, or feel things that are not present, or they may experience a distortion of their senses.
Paranoia or suspiciousness: The person may become paranoid or suspicious of others, even if they were previously familiar with them.
Physical symptoms: The person may experience physical symptoms such as sweating, shaking, or rapid heartbeat.
If you observe any of these signs, it is crucial to stay calm and offer reassurance to the person. However, if the symptoms worsen or persist, it is essential to seek medical attention immediately.
Reassurance and supportive care

Reassurance and supportive care are important aspects of managing a bad trip. They involve creating a safe and calming environment for the person experiencing the bad trip, and providing emotional support and reassurance to help them manage their symptoms.
Remember that reassurance and supportive care are not a substitute for professional medical help, especially in cases where the person is experiencing severe symptoms or is at risk of harm. Here are some structured details on how to provide reassurance and supportive care:
Move the person to a safe space

Moving the person to a safe space or creating a safe environment during a bad trip is crucial for their well-being. When choosing a safe space, it’s important to consider the following:
Comfort: The space should be comfortable and familiar to the person, which can help to reduce anxiety.
Privacy: The person should be able to have some privacy, away from the noise and distractions of others.
Safety: The space should be free from hazards or objects that could cause harm (sharp objects, open fire, balcony or open window, transport).
Calm environment: The space should be quiet and peaceful, without crowd, bright lights or loud noises. All these intense external stimuli can cause severe symptoms and accelerate the Bad Trip train.
To move the person to a safe space, follow these steps:
- Stay calm and reassure the person that you are there to help.
- Gently guide the person to a quiet, calm, and familiar location. Avoid sudden movements or loud noises that may exacerbate their anxiety.
- Sit with the person and offer reassurance. Talk calmly and softly, and let them know that they are safe.
- If possible, dim the lights, turn off any loud music or TV, and provide a comfortable place to sit or lie down.
Some suitable places for a safe space during a bad trip include a bedroom, a quiet outdoor space, or a quiet room with comfortable seating. It’s essential to avoid overcrowded areas, loud environments, or unfamiliar locations, which can exacerbate anxiety and increase the risk of harm.
Remind the person that the feeling will wear off

Reminding the person that the feelings during a bad psychedelic trip will wear off can help to reduce their anxiety and provide reassurance. Here are some tips for doing so in a safe and effective manner:
Speak calmly and reassuringly: Use a calm and soothing tone when speaking to the person. Reassure them that what they are experiencing is temporary and that it will pass.
Use simple and straightforward language: Avoid using complex language or medical terminology that could confuse or agitate the person.
Repeat your message: It can be helpful to repeat your message several times, as the person may be having difficulty processing information.
Avoid making false promises: While it’s essential to reassure the person that they will be okay, avoid making false promises or guarantees that could make the situation worse.
Avoid confrontation or judgment: Avoid arguing with the person or telling them that their experience is not real. Instead, try to validate their feelings and experiences and provide a non-judgmental and accepting attitude.
Provide distractions: Providing distractions, such as quiet ambient chill music or a calming activity, can help to take the person’s mind off their anxiety and allow them to relax.
Offer support: Let the person know that you are there to help and that you will stay with them until they feel better. Let them know that they are safe. Encourage them to focus on their breathing and try to stay relaxed.
Provide physical comfort: Offer the person a glass of water or a blanket to help them feel more comfortable. Physical touch such as a gentle hand on the shoulder or holding their hand can also be reassuring, but it’s important to ask for their consent before doing so.
It’s important to remember that everyone’s experience with a bad trip is different, and what works for one person may not work for another.
Stay with the person at all times

Staying with a person at all times during a bad trip is crucial for their safety and well-being. However, it’s also important to take steps to ensure your own safety. Here are some tips for staying with the person safely during a bad trip:
Stay calm: Maintaining a calm and reassuring presence can help to reduce the person’s anxiety and prevent the situation from escalating.
Be aware of your surroundings: Take note of any potential hazards in the environment, such as sharp objects or tripping hazards, and move them out of reach if possible.
Avoid physical contact: If the person is agitated or aggressive, avoid physical contact that could escalate the situation. Instead, try to speak to them calmly and provide reassurance from a safe distance.
Have a plan in place: Before the bad trip occurs, have a plan in place for what to do in case of an emergency. This can include knowing the location of the nearest hospital or emergency services.
Consider enlisting the help of others: If possible, enlist the help of others to stay with the person. This can provide additional support and help to ensure everyone’s safety.
Take breaks if needed: If you feel overwhelmed or need to take a break, it’s okay to do so. Ensure that someone else is there to take your place and stay with the person.
Overall, staying with a person during a bad trip requires a calm and level-headed approach, as well as taking necessary safety precautions to ensure both you and the person are safe.
Stay safe and protect others

During a bad trip, it’s important to prioritize safety for both the person experiencing the trip and those around them.
Limit the number of people present: Too many people in the immediate area can increase anxiety and make the situation worse. Limit the number of people present to those who are calm and can help support the person.
Call for medical help if needed: If the person is showing signs of severe distress or appears to be in danger, call for medical help immediately. A healthcare professional can provide additional support and guidance for managing a bad trip.
Overall, staying safe and protecting others during a bad trip requires a calm and level-headed approach, as well as taking necessary safety precautions to ensure everyone’s well-being.
Get medical or other professional help if needed

Unfortunately, even considering the reversible nature of a Bad Trip, it can always develop into something more serious and reach the level of a Psychotic Disorder. If you see that all measures do not help, the person’s condition worsens or a very long time has passed (tens of hours) without explicit stabilization, the best solution would be to turn to professionals.
Call emergency services: In cases of severe distress or danger, call emergency services (such as 911 in the US) immediately. A healthcare professional can provide immediate medical attention and support.
Contact a mental health professional: If the person is experiencing ongoing distress or symptoms after the bad trip, consider contacting a mental health professional. This can include a therapist, psychologist, or psychiatrist.
Contact a crisis helpline: There are several crisis helplines available that can provide support and guidance during a bad trip. These services are often staffed by trained professionals who can provide advice on managing symptoms and finding additional resources.
Go to the emergency room: If the person is experiencing severe symptoms or appears to be in danger, take them to the nearest emergency room. Healthcare professionals can provide immediate medical attention and support.
It’s important to remember that seeking professional help is not a sign of weakness, and can be a critical step in managing a bad trip and preventing further harm. If you or someone you know is experiencing a bad trip and needs professional help, don’t hesitate to reach out for support.
Conclusion

The first aid for a bad trip includes recognizing the signs of a bad trip, moving the person to a safe space, reassuring them that the effects will wear off, and staying with them at all times while prioritizing safety for both the person and others around them. If necessary, seek professional help through emergency services. Remember to stay calm, take necessary safety precautions, and prioritize the well-being of the person experiencing the bad trip.
Being prepared to help someone who is experiencing a Bad Trip is essential. By following these first-aid steps, you can provide the necessary support to help the individual feel safe and calm and ensure that they receive the appropriate care and they will not find themselves alone with the unfolding state of psychosis, from which no one is protected.