Hallucinogen Persisting Perception Disorder (HPPD) is a condition characterized by the recurrence of perceptual symptoms that were previously experienced during acute hallucinogen intoxication, even after the drug has ceased to be active in the system. These symptoms can manifest as visual disturbances or hallucinations.
In addition to the name mentioned, this condition may occur under the name Hallucinogen Use Disorder (HUD). This is not entirely accurate, because HUD can include HPPD, but is not limited to it, including other hallucinogen related disorders. However, I will use both names, meaning in this article it is HPPD and no other state.
The exact prevalence of HPPD is unknown. It’s noteworthy that despite millions of hallucinogen users since the 1960s and 1970s, there have been relatively few published case reports of HPPD. However, every year this condition is heard more and more often, and it can be considered not only as a negative effect of hallucinogens but also a characteristic condition for other substances. I think the name may change in the future.
Mechanisms of Hallucinogen Use Disorder
The exact mechanisms underlying HPPD remain elusive, but several studies have attempted to shed light on its pathophysiology:
Etiological Factors
- Drug Induction: HPPD is closely linked to the consumption of hallucinogenic drugs. Common drugs associated with HPPD include lysergic acid diethylamide (LSD), 3,4-Methyl enedioxy methamphetamine (MDMA), and cannabinoids. We will discuss this in more detail below.
- Individual Susceptibility: While the prevalence of HPPD is low, it is more often diagnosed in individuals with a history of psychological issues or substance misuse. However, it can manifest in anyone, even after a single exposure to triggering drugs.
Neurological Mechanisms
- Delta Oscillations: One study on a 33-year-old male patient with HPPD symptoms found increased delta activity over the occipital brain regions during a 32-channel electroencephalography (EEG) assessment. This delta activity was reminiscent of occipital intermittent rhythmic delta activity (OIRDA) typically observed in children. The study suggested that pathological delta activity in the occipital brain regions might play a crucial role in the development and perpetuation of HPPD.
Comorbidities:
- HPPD can coexist with other conditions. For instance, one study investigated the prevalence of migraine in individuals with HPPD presenting as visual snow syndrome (VSS)4.
While the exact mechanisms of HPPD remain a topic of ongoing research, it is evident that neurological factors, individual susceptibility, and the type of hallucinogenic drug consumed play a role in its manifestation. Further research is needed to fully understand the pathophysiology and develop effective treatment strategies.
What Drugs Can Cause HPPD?
Migraine prevalence in visual snow with prior illicit drug use…
Despite the fact that we do not fully know the etiology of the pathogenesis of HPPD, these types of drugs cause distortion of perception and other symptoms of the condition more often than others:
- Lysergic Acid Diethylamide (LSD): LSD is a potent hallucinogenic drug that can lead to HPPD. It mediates its hallucinogenic effects mainly via activating the serotonergic 5HT2a-receptor.
- 3,4-Methyl enedioxy methamphetamine (MDMA): MDMA, commonly known as ecstasy, is another drug associated with HPPD. It’s often used recreationally for its euphoric effects.
- Cannabinoids: Cannabinoids, including marijuana, have been linked to HPPD. In some cases, cannabinoids and MDMA were used in association with classical hallucinogens.
- While traditional cannabinoids like marijuana have been linked to HPPD, synthetic cannabinoids, often sold as “Spice” or “K2,” have also been associated with the disorder. These synthetic drugs can have unpredictable and severe effects.
- Psilocybin (Magic Mushrooms): Psilocybin, the active compound in magic mushrooms, can induce hallucinations and altered perceptions. Magic mushrooms trip simulation is not you need to worry about, but HPPD from mushrooms occurs quite often.
- Mescaline (Peyote): Mescaline is the active compound in the peyote cactus and is known for its hallucinogenic properties. Like other hallucinogens, mescaline can lead to the development of HPPD in some users.
- Dimethyltryptamine (DMT): DMT is a powerful hallucinogenic drug found in certain plants and animals. It can induce intense visual and auditory hallucinations. Some users have reported HPPD symptoms after DMT use.
- Phencyclidine (PCP or Angel Dust): PCP is a dissociative drug that can cause hallucinations, distorted perceptions, and feelings of detachment. It’s also been associated with HPPD in some cases.
- Ayahuasca: Ayahuasca is a traditional South American brew that contains DMT. It’s used in religious and shamanic rituals. Some individuals have reported persistent visual disturbances after participating in Ayahuasca ceremonies.
- Salvia divinorum: Salvia is a plant that can induce intense, short-lived hallucinations. Some users have reported HPPD-like symptoms after using Salvia.
- Citalopram: Citalopram, an antidepressant belonging to the selective serotonin reuptake inhibitors (SSRI) class, has been reported to induce visual snow syndrome, which shares symptoms with HPPD. There are reports of visual sensations arising years after LSD abuse triggered by the intake of SSRIs in patients with former HPPD.
Symptoms of Hallucinogen Use Disorder
First, I will give the free signs collected by me. And then I will focus on the official diagnostic criteria. Let’s delve into the symptoms of hallucinogenic drug perception disorder:
- Visual Disturbances:
- Visual Snow: This is a continuous visual disturbance where individuals see what looks like “static” or “TV snow” in their visual field.
- Floaters: These are small moving spots that appear in one’s field of vision. They may appear as black or gray specks, strings, or cobwebs that drift about when the eyes are moved.
- Afterimages (Palinopsia): This refers to the persistence of images after the visual stimulus has been removed. For example, if someone looks at a light and then looks away, they might still see the light for a prolonged period.
- Tracers: These are streaks that follow moving objects in one’s field of vision.
- Halos Around Objects: This symptom involves seeing bright circles around light sources or objects.
- Starbursts: Seeing rays or bursts of light coming out from light sources.
- Intensified Colors: Some individuals report that colors appear more vibrant or intense than usual.
- Photophobia: This is an increased sensitivity to light. Individuals with photophobia may find bright lights or even normal daylight to be too intense and uncomfortable.
- Nyctalopia (Night Blindness): Difficulty or inability to see in low-light conditions or at night.
- Geometric Hallucinations: Seeing patterns, shapes, fractals, or other psychedelic visuals that aren’t present.
- Derealization and Depersonalization: These are forms of dissociative symptoms. Derealization involves feeling that the external world is strange or unreal, while depersonalization involves feeling detached from oneself.
- Auditory Symptoms: Although less common, some individuals report auditory disturbances, such as hearing sounds that aren’t present.
- Tactile Hallucinations: Feeling sensations on the skin that aren’t caused by any external stimuli, such as tingling, burning, or itching.
- Anxiety and Panic Attacks: Many individuals with HPPD experience heightened anxiety, which can sometimes lead to panic attacks.
- Mood Disturbances: This can include symptoms of depression, irritability, or other mood changes.
- Impaired Concentration: Some individuals report difficulty focusing or concentrating on tasks.
It’s important to note that the symptoms of HPPD can vary in intensity and frequency among individuals. Some may experience constant symptoms, while others might have intermittent episodes. Additionally, the presence of these symptoms, especially in the absence of recent drug use, can be distressing and lead to significant impairment in daily functioning.
DSM-5 Diagnostic Criteria for HPPD
- Criterion A: Following cessation of use of a hallucinogen, the reexperiencing of one or more of the perceptual symptoms that were experienced while intoxicated with the hallucinogen. This includes:
- Geometric hallucinations
- False perceptions of movement in the peripheral visual fields
- Flashes of color
- Intensified colors
- Trails of images of moving objects
- Positive afterimages
- Halos around objects
- Macropsia (seeing objects larger than they are) and micropsia (seeing objects smaller than they are).
- Criterion B: The symptoms in Criterion A cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- Criterion C: The symptoms are not attributable to another medical condition (e.g., anatomical lesions and infections of the brain, visual epilepsies) and are not better explained by another mental disorder (e.g., delirium, major neurocognitive disorder, schizophrenia) or hypnopompic hallucinations.
ICD Criteria for HPPD
I could not find clear criteria and even something similar in description to the CPP with any specifics in the latest edition of the ICD-11. The only subsections and codes where we can write the HPPD are:
- 6C49.Y Other specified disorders due to use of hallucinogens
- 6C49.Z Disorders due to use of hallucinogens, unspecified
Chapter 6C49.6 Certain specified hallucinogen-induced mental or behavioral disorders сontains only criteria for mood disorder and anxiety disorder. It doesn’t suit us. I hope that perception disorder will be added here in the future. It’s funny that in ICD-10 there was a diagnosis of Flashback – the condition closest to HPPD for diagnostic. It’s strange that I can’t find it in the new edition of the manual. Or maybe I was looking badly.
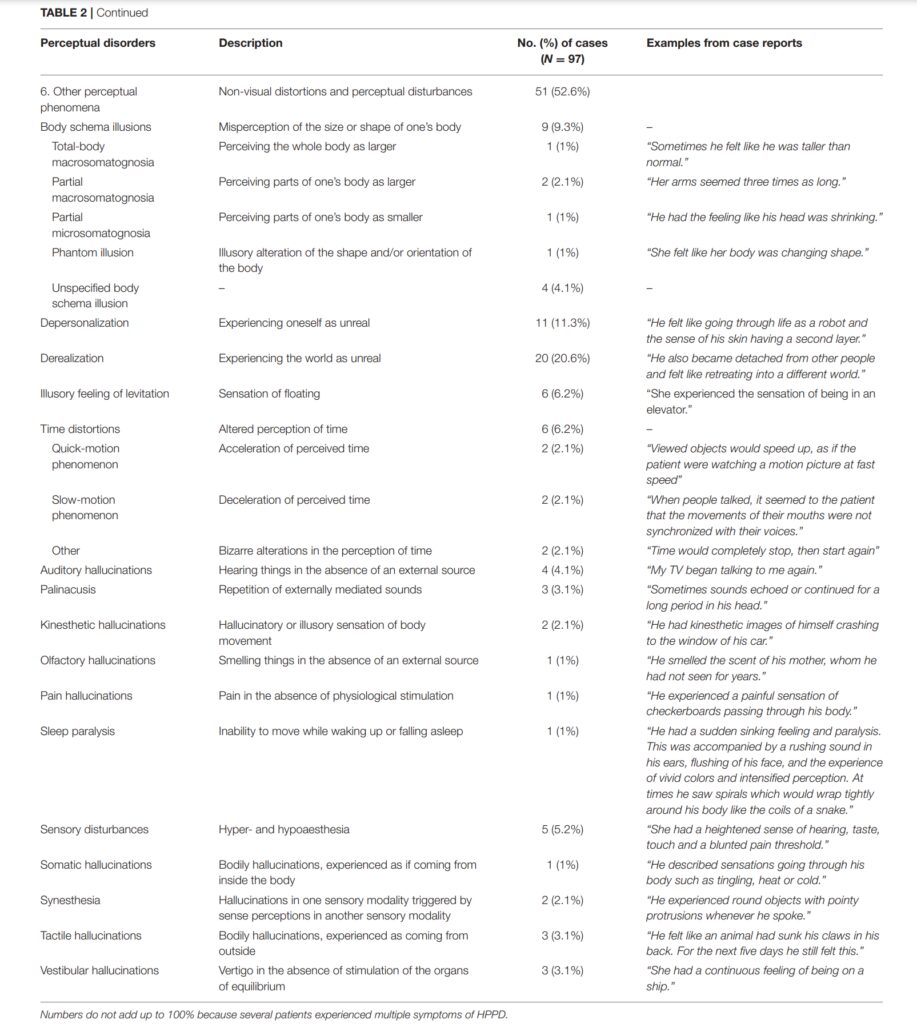
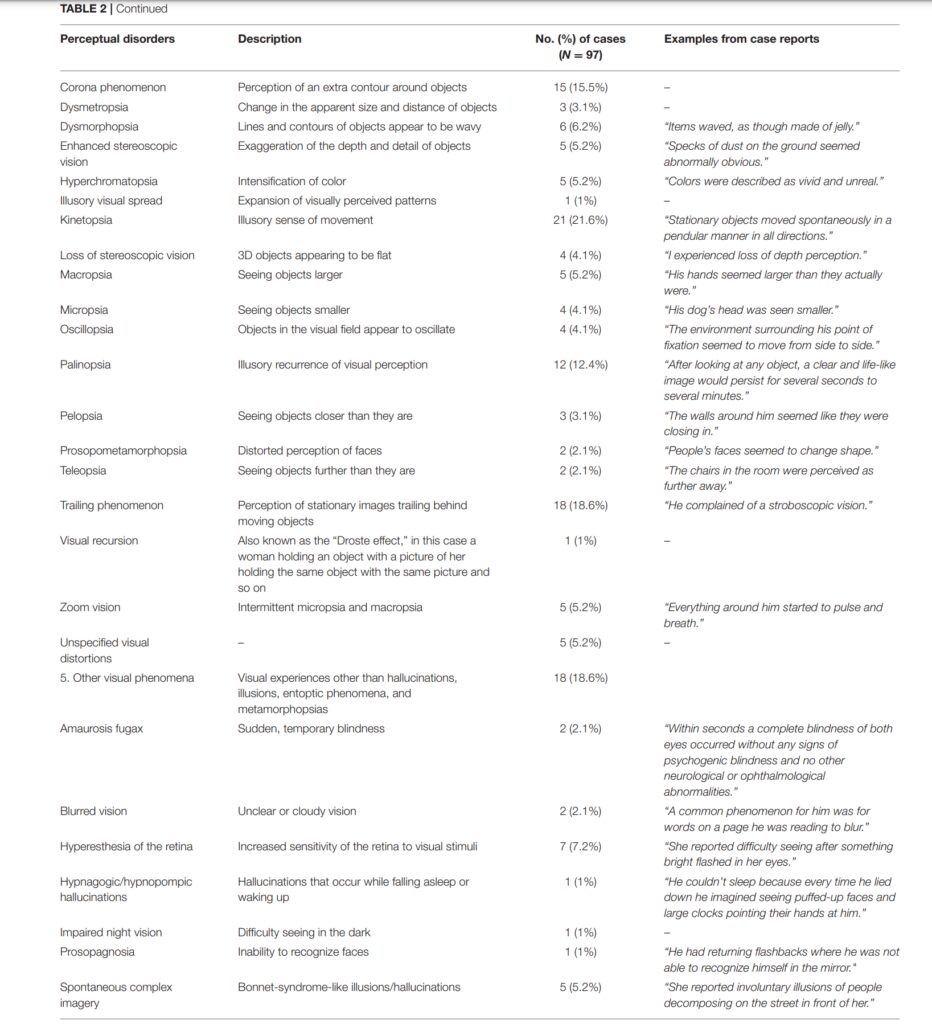
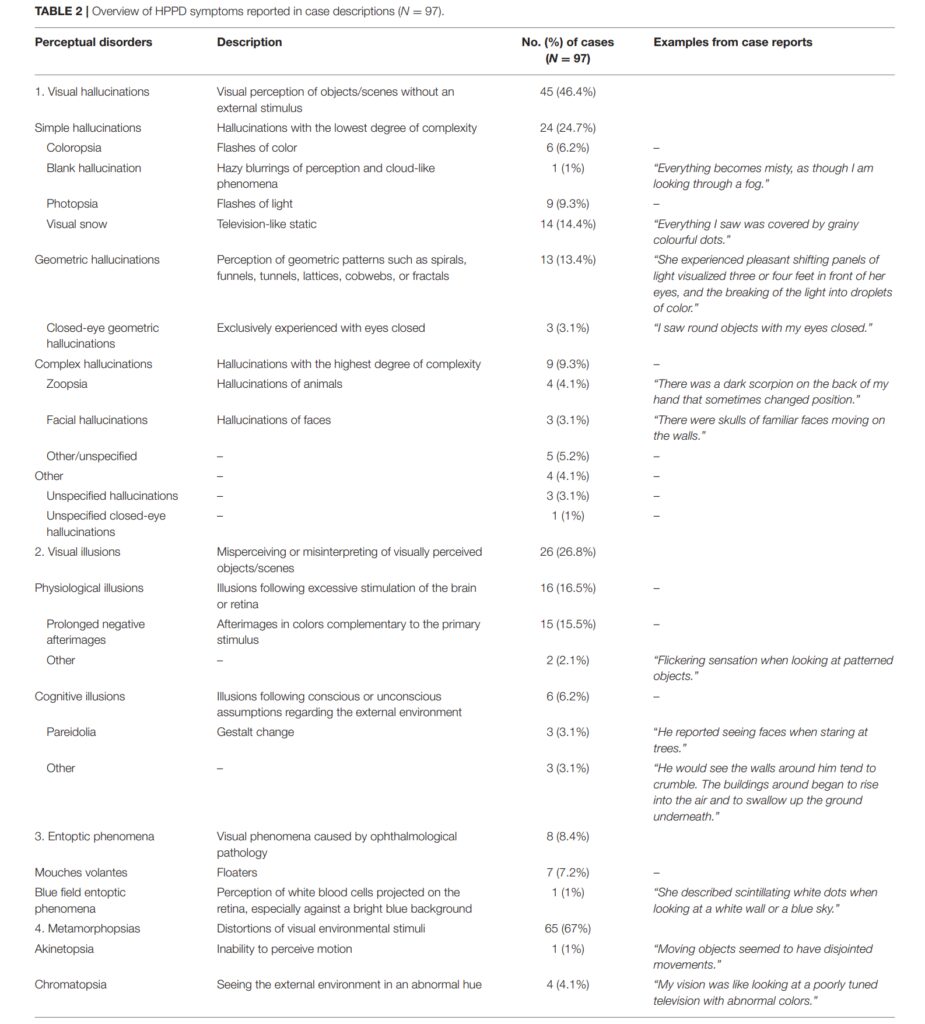
On Perception and Consciousness in HPPD: A Systematic Review
Anyway, I urge readers not to engage in self-diagnosis and self-medication, especially if the hallucinogenic pictures and other symptoms bring serious problems and interfere with life. Contact medical professionals for help.
Types of HPPD and Flashbacks
Type 1 HPPD
First type involves brief re-experiences of alterations in perception, mood, and/or consciousness, similar to those experienced during a hallucinogenic intoxication. These experiences are characterized by their brevity, infrequency, and intermittency, and are often referred to as flashbacks.
The course of the HPPD I is typically mild, non-troubling, and confined in both time span and seriousness. Medical treatment may be necessary, but the outcomes are generally very good.
Type 2 HPPD
Thise entitie involves constant or near-constant visual effects. These effects can include various symptoms. Some individuals fail to acclimate to the presence of these persistent, recurring visual and sensory disturbances. Symptoms may occur alone or in combination, and while sound and other perceptions are typically unaffected, they are often reported as uncontrollable and disturbing. However, some individuals may regard them as enriching. Claimed constant visual phenomena are often accompanied by mild-to-moderate depersonalization, derealization, anxiety, or depression, and these psychopathological states are thought to trigger the occurrence and intensity of visual phenomena. There is a consistent subgroup within those individuals with HPPD II that necessitates continual pharmacologic intervention.
Are Flashbacks Hallucinations?
Flashbacks can occur weeks, months, or even years after the initial drug experience and may be pleasurable and controllable. They typically manifest as visual increases in perceived color intensity, dimensionality, or vibrancy; illusory changes; and/or movement of a perceived object. Alterations in the perception of time may also occur, and strong emotions felt during the drug experience may recur. In some cases, ego boundaries can become diffuse.
Flashbacks can be distinguished from psychotic disorders by their episodic nature, often lasting only seconds or minutes, and by their duplication of previous drug-related experiences. Relevant reviews have concluded that these experiences are usually self-limited and diminish in duration, intensity, and frequency over time.
It’s essential to differentiate between flashbacks and HPPD. While flashbacks are brief and can be pleasant, HPPD is more persistent and can cause significant distress.
There are other conditions, such as Afterglow and Alice in Wonderland Syndrome. In my opinion, all of them can be both partial manifestations and components of our main character – HPPD.
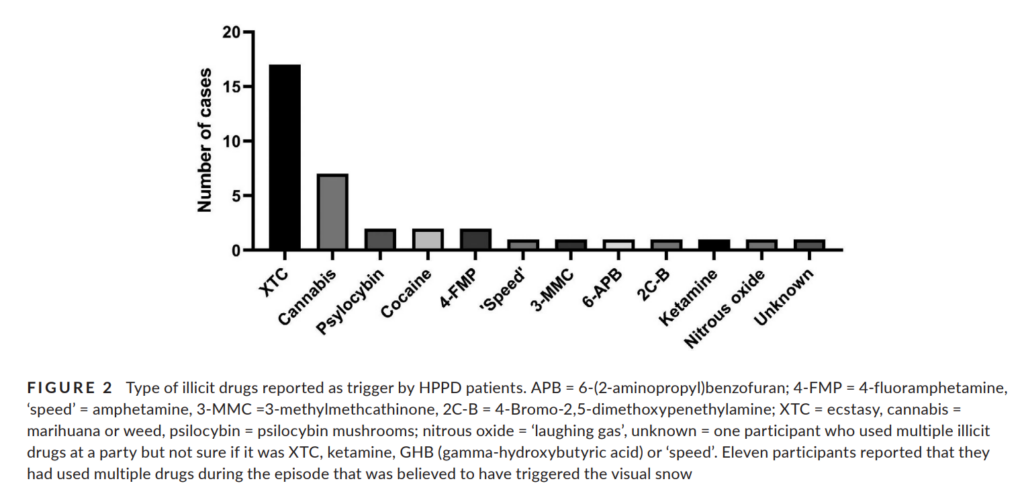
Triggers for Psychedelic Visual Disorder
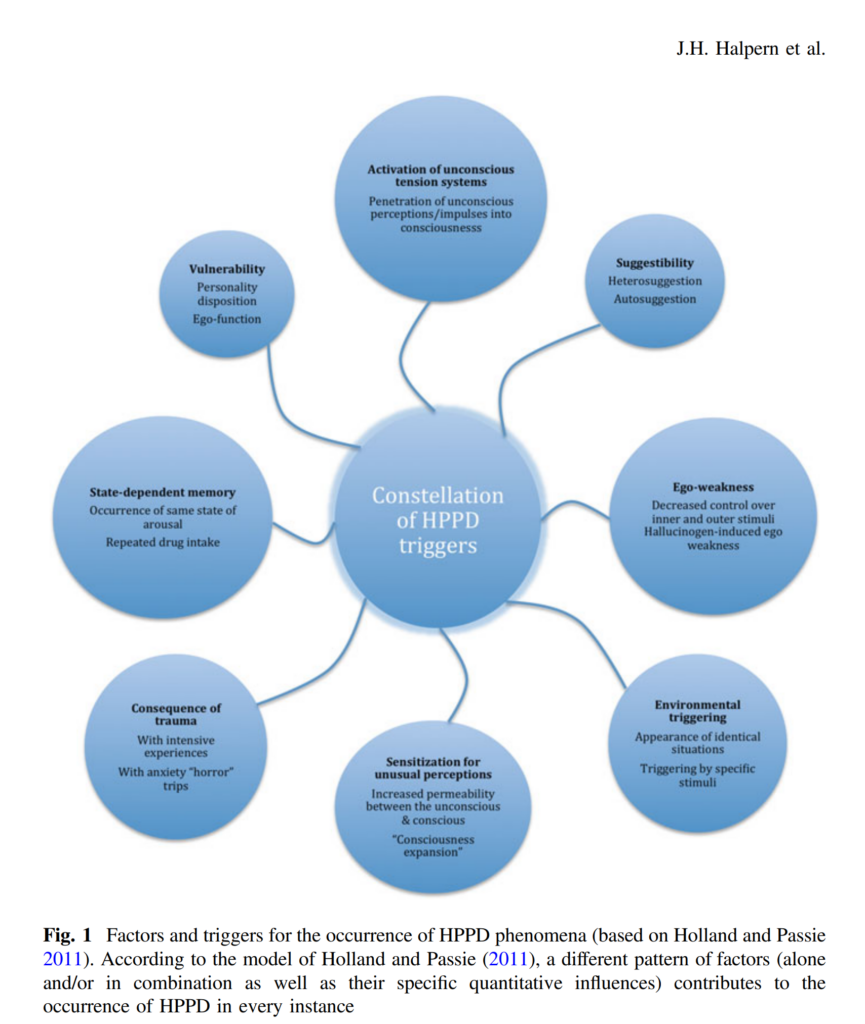
Hallucinogen Persisting Perception Disorder: Etiology, Clinical Features, and Therapeutic Perspectives
Here I will just leave an image with a link to the source that is excellent in content and clarity. I have nothing to add.
HPPD Recovery and Treatment
Data on HPPD recovery and treatment are still fragmentary, isolated, and do not add up to an objective scheme. Somewhere insufficient, somewhere redundant, somewhere completely experimental methods are used. We have yet to learn how to deal with this condition. Here’s what I managed to collect:
- Medical Consultation: If you suspect you have HPPD, it’s crucial to consult with a healthcare professional to get a proper diagnosis and rule out other potential causes for the symptoms.
- Avoid Drug Use and Other Triggers: Refraining from further use of hallucinogens or other recreational drugs can help prevent exacerbation of symptoms.
- Support: Joining support groups or seeking counseling can help individuals cope with the distress caused by HPPD.
- Treatment Options: While there’s no standardized treatment for HPPD, some therapeutic approaches have been explored.
- Positive effects of psychotherapy are reported. Anxiety reduction, muscle relaxation, and reframing one’s visual phenomena through personal destigmatization and normalization may be beneficial. Cognitive behavioral therapy (CBT) has shown promise for somatic symptom disorders, as well as related distress from tinnitus. CBT has also shown promise for depersonalization-derealization disorder, which frequently co-occurs with HPPD.
- Also, a visual snow sensory intervention involving online delivery of staring at static gives hope.
- A pilot study, which is more than 20 years old, has shown that Clonidine, an antihypertensive agent, can reduce the severity of flashbacks after using LSD
- Of the drugs, benzodiazepines (lorazepam, clonazepam), SSRIs (escitalopram) and SNRI (serotonin-norepinephrine reuptake inhibitors show) some effectiveness.
- Some reduction of symptoms was achieved with the help of anticonvulsant drugs like lamotrigine, gabapentin, levetiracetam and valproic acid.
- Atypical antipsychotics (aripiprazole or risperidone) in some cases helped to completely neutralize the symptoms. However, the reasons for their use should be really good.
- One study explored the therapeutic potential of non-invasive brain stimulation. Two sessions of cathodal (inhibitory) transcranial direct current stimulation (tDCS) over 30 minutes reduced the visual hallucinations and occipital delta activity by approximately 60%, with the response lasting for over four weeks.
Conclusion

HPPD is a complex and not fully understood condition. We have been observing it for a long time, but we have not fully understood it, and have not developed a single view and algorithm of treatment.
At the same time, many people today present symptoms characteristic of HPPD and this number will only grow. Gradually, doctors and consumers should come to understand that the long-term consequences of using classical psychedelics and other substances deserve special attention because a person finds themself in a situation where they were able to give up the substance, go a long way, but before changes in the neurochemistry of the brain, as well as triggers, do not allow they to completely free thyself from the action of substances.
Everyone should know about it. This should be understood when making a choice regarding the use of a substance. Making choices during diagnosis and treatment selection. Holding a consultation and starting a party. This can affect many of us and our loved ones.