What is an opioid overdose?
An opioid overdose occurs when an individual takes an excessive amount of opioids, such as prescription painkillers (e.g., oxycodone, hydrocodone) or illicit substances like heroin or fentanyl. Opioids are potent pain-relieving medications that affect the central nervous system.
Why can an opioid overdose cause death? So, when opioids are taken in high doses, they can depress the respiratory center in the brainstem, which controls breathing. This leads to a decrease in the rate and depth of breathing, and in severe cases, it can cause respiratory arrest, where breathing completely stops. As a result, oxygen supply to the body decreases, and carbon dioxide levels rise, leading to a cascade of harmful effects.
Risk factors for opioid overdose

Several risk factors can contribute to an increased likelihood of opioid overdose. It is important to be aware of these factors to identify individuals who may be at higher risk and take appropriate preventive measures. Here are some key risk factors:
High-dose or long-term opioid use
Taking higher doses of opioids or using them for an extended period increases the risk of developing tolerance and strong addictive behavior, which can lead to accidental overdose.
Tolerance refers to the body’s ability to process a specific drug. A person with low tolerance requires a smaller amount of a drug to experience its effects, while someone with increased tolerance needs higher doses.
Tolerance develops over time, meaning long-term users require larger amounts of a drug to achieve the desired effects compared to newer users. Tolerance can fluctuate based on factors such as weight, size, illness, stress, compromised immune system, and age.
Notably, tolerance can decrease rapidly after a period of abstinence, whether intentional (e.g., during drug treatment or methadone detox) or unintentional (e.g., due to incarceration or hospitalization). Research also suggests that tolerance is affected when drugs are used in a new or unfamiliar environment, putting individuals at a higher risk of overdose.
Concurrent use of multiple substances
When different drugs are taken together, they can interact in ways that amplify their overall effects. Many overdoses occur when heroin or prescription opioids, alcohol, and benzodiazepines like Klonopin, Valium, and Xanax are mixed. The majority of fatal overdoses result from using multiple drugs simultaneously.
Sedating medications individually carries overdose risks. However, when combined, the risk is significantly increased because these drugs affect the body’s sedation mechanisms in different ways. These mechanisms provide overlapping protection for the brain and respiration. Combining multiple substances diminishes this overlapping protection, meaning that even a smaller amount of heroin can cause an overdose when there are higher levels of alcohol and/or downers present in the system.
Speedballing, which involves mixing heroin and cocaine, is another common drug combination. Despite the assumption that the stimulant and depressant effects would counterbalance each other, the risk of overdose remains high for speedball users. This is likely due to factors such as increased drug processing by the body, the stimulant’s effect on oxygen usage, the depressant’s impact on breathing rate, and the frequency of injection among speedball users.
Previous overdose
A history of prior opioid overdose is a significant risk factor for future overdoses. Surviving an overdose does not guarantee immunity from future incidents, and subsequent episodes may be even more dangerous.
Lack of familiarity with opioids
Individuals who are not familiar with opioid medications, their potency, or safe use practices may be at higher risk of unintentional overdose. This includes individuals who may come into contact with opioids through prescription use, sharing medications, or using illicit drugs.
Opioid potency and source
The use of illicitly manufactured opioids, particularly fentanyl and its analogs, has contributed to a significant increase in overdose deaths. These potent synthetic opioids may be mixed with other drugs, making it challenging for individuals to know the exact contents and dose, thereby increasing the risk of overdose.
The term “quality” refers to the purity and strength of a drug. Street drugs are often unpredictable in terms of content and purity. They may be adulterated with other substances that pose additional dangers. Assessing the purity of drugs visually is not possible, and purity levels can vary, resulting in unexpectedly strong doses that increase the risk of overdose.
Prescription drugs also pose risks. While the contents and dosages of pills are known, the strength can still differ between different types of medications within the same opioid family (e.g., OxyContin vs. Vicodin). Understanding the strength and dosage of both street drugs and prescription medications is crucial for avoiding overdose.
Mental health conditions
Co-occurring mental health disorders, such as depression, anxiety, or post-traumatic stress disorder (PTSD), can increase the risk of opioid overdose. These conditions may lead to self-medication with opioids, resulting in higher doses or misuse.
Age and gender
Certain age groups and genders may be at higher risk. Middle-aged adults (25-54 years old) have shown higher rates of opioid overdose deaths compared to other age groups. Men have historically had higher rates of opioid overdose, although recent years have seen an increase in overdose rates among women as well.
Age and physical health significantly influence the body’s ability to handle drugs. Older individuals and those with prolonged histories of drug use are at higher risk of fatal overdose. While experience with substances can be somewhat protective, long-term substance use, coupled with conditions like viral hepatitis, HIV/AIDS, or infections such as endocarditis or cellulitis, can reduce resilience. Older individuals who overdose are less likely to survive compared to younger individuals. Compromised immune systems, recent illnesses, or weakened states increase the risk of overdose. Dehydration, lack of eating or sleeping also elevate the risk.
Stimulant users with additional health issues like high blood pressure, heart disease, diabetes, high cholesterol, or smoking are at higher risk of experiencing seizures, strokes, or heart attacks.
A recent release from incarceration
Individuals who have recently been released from correctional facilities face an increased risk of overdose due to factors such as a reduced tolerance to opioids, difficulty accessing treatment and support services, and exposure to high-risk environments.
Social isolation and stigma
Social isolation, lack of support networks, and the presence of Stigma surrounding opioid use can contribute to increased risk. These factors may deter individuals from seeking help, limit access to resources, and increase the likelihood of using opioids in unsafe or unsupervised environments.
While using drugs alone does not directly cause overdose, it significantly increases the likelihood of a fatal overdose. If an overdose occurs when someone is alone, there is no one present to call for help or provide immediate assistance. Many fatal overdoses have been discovered in closed or locked spaces, preventing intervention.
It is important to note that having one or more risk factors does not mean an individual will experience an overdose. However, recognizing these factors can help identify individuals who may benefit from targeted interventions, such as education, harm reduction strategies, and appropriate treatment options for substance use disorder.
Symptoms & Signs of opioid overdose
Opioid overdose symptoms can vary, but some common indicators include:
- Slow or shallow breathing: Opioids can depress the respiratory system, causing breathing to become slow, irregular, or even stop altogether.
- Extreme drowsiness or unresponsiveness: Opioid overdose can lead to severe sedation, making it difficult for the affected person to stay awake or respond to stimuli.
- Pinpoint pupils: One characteristic sign of opioid overdose is constricted or pinpoint pupils, where the black center of the eye appears very small.
- Pale or clammy skin: Due to decreased blood flow, the skin may become pale, cool, and sweaty to the touch.
- Bluish lips or nails: Lack of oxygen can result in a bluish or purplish discoloration of the lips, face, or nail beds.
- Slow heart rate: Opioids can lower heart rate, leading to bradycardia, where the pulse is unusually slow.
If you suspect someone is experiencing an opioid overdose, it is crucial to seek immediate medical help by calling emergency services.
Emergency Responses to Opioid Overdose

When responding to an opioid overdose, it is crucial to take immediate action. Here are the recommended emergency responses and treatments for opioid overdose:
- Call emergency services: Dial the emergency number in your country (such as 911 in the United States) to request immediate medical assistance. Provide clear and accurate information about the situation, including the possibility of an opioid overdose.
- Stay with the person: Do not leave the individual alone, as their condition can deteriorate rapidly. Stay by their side to monitor their vital signs and provide reassurance until medical help arrives.
- Administer naloxone if available: If you have access to naloxone, follow the instructions provided with the medication and administer it promptly. Naloxone is available as an injectable medication or as a nasal spray. It can reverse the effects of opioid overdose by blocking the opioid receptors in the brain, restoring normal breathing and consciousness.
- Support their breathing: Ensure that the person’s airway is clear and open. If they are not breathing or have shallow breathing, perform rescue breaths by giving mouth-to-mouth resuscitation. If you are trained in cardiopulmonary resuscitation (CPR), you may also initiate chest compressions if needed.
- Stay on the line with emergency services: If you called emergency services, remain on the line to provide any necessary updates or receive further instructions from the dispatcher. They may be able to provide guidance on how to perform CPR or other life-saving measures if needed.
Remember, time is critical during an opioid overdose. By promptly seeking professional medical help and administering naloxone if available, you can significantly improve the chances of a positive outcome.
Learn more about First Aid for Opioid Overdose
Prevention of opioid overdose

Preventing opioid overdose involves various strategies aimed at reducing the risk of overdose and promoting safer opioid use. Here are some key preventive measures:
Education and awareness: Public education campaigns play a vital role in raising awareness about the risks associated with opioid use and overdose. Educating individuals about the signs of opioid overdose, proper medication use, and the importance of seeking help for substance use disorders can help prevent overdoses.
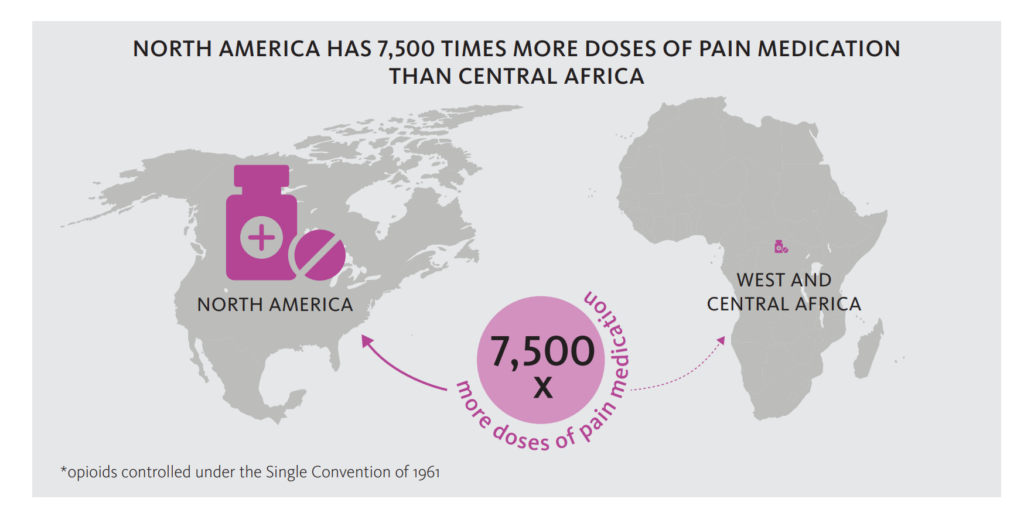
Prescription guidelines and monitoring: Healthcare providers should follow evidence-based guidelines when prescribing opioids, including assessing the patient’s risk for substance misuse, using the lowest effective dose, and considering non-opioid alternatives for pain management whenever possible. Regular monitoring and communication with patients can help identify any misuse or signs of dependence.
Naloxone availability and training: Naloxone is a life-saving medication that can rapidly reverse opioid overdose. Expanding access to naloxone and providing training on its administration to healthcare professionals, first responders, individuals at risk of overdose, and their family members can significantly reduce overdose deaths.
Medication-assisted treatment (MAT): MAT combines medications like methadone, buprenorphine, or naltrexone with counseling and behavioral therapies. It is an evidence-based approach for treating opioid use disorders, reducing cravings, and decreasing the risk of overdose. Expanding access to MAT and reducing barriers to treatment are critical in preventing overdoses.
Harm reduction strategies: Harm reduction approaches aim to minimize the negative consequences of drug use without necessarily requiring abstinence. Examples include needle exchange programs, safe injection sites, and providing information on safer drug use practices. These strategies can help reduce the risk of overdose and the transmission of infectious diseases.
Support and treatment services: Ensuring that individuals have access to comprehensive support and treatment services for substance use disorders is crucial. This includes counseling, therapy, support groups, and rehabilitation programs tailored to meet the specific needs of individuals struggling with opioid use.
Responsible medication disposal: Proper disposal of unused or expired medications can help prevent accidental or intentional misuse. Follow local guidelines or participate in drug take-back programs to ensure safe disposal of opioids.
Prevention of opioid overdose requires a multifaceted approach involving education, policy changes, access to treatment, and support services. By implementing these strategies, we can work towards reducing the incidence of opioid overdose and promoting safer opioid use practices.
Statistics of opioid overdoses in the United States
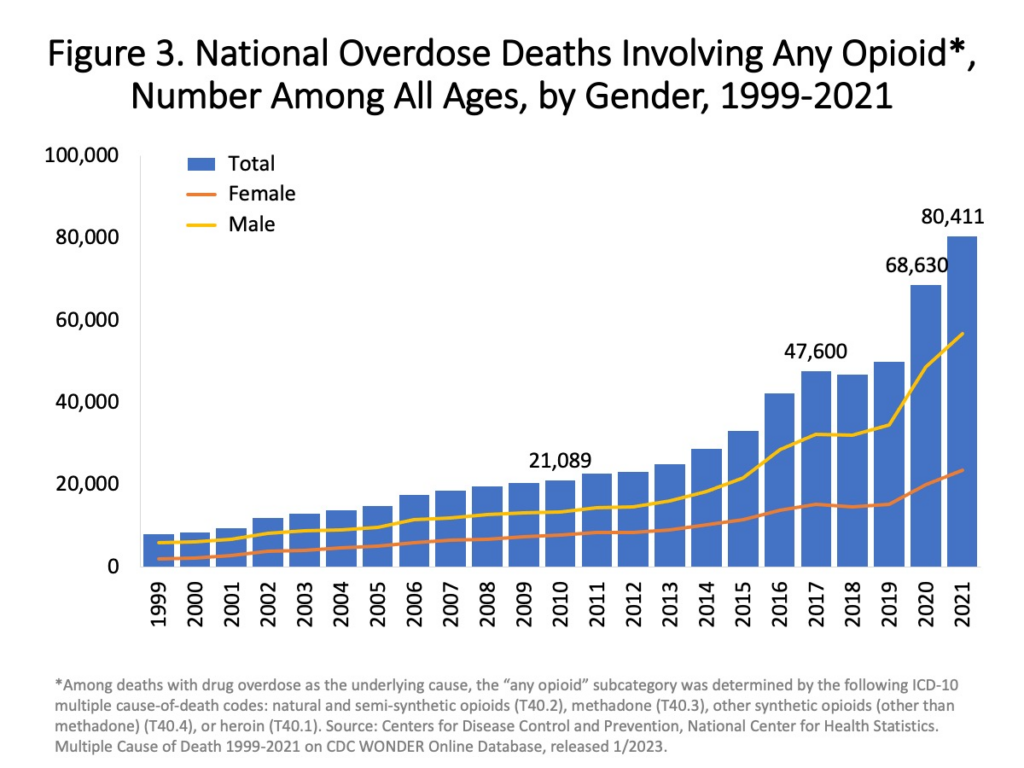
Here are some key opioid overdose statistics related in the United States according to the Centers for Disease Control and Prevention (CDC) or the National Institute on Drug Abuse (NIDA).
Opioid overdose deaths: In recent years, the United States has been facing a significant opioid crisis. According to CDC data, in 2019, there were over 49,000 opioid overdose deaths, which accounted for nearly 70% of all drug overdose deaths in the country.
Prescription opioids vs. synthetic opioids: Prescription opioids, such as oxycodone and hydrocodone, were initially major contributors to the opioid crisis. However, in recent years, synthetic opioids, particularly illicitly manufactured fentanyl, have been increasingly involved in overdose deaths. Fentanyl is estimated to be 50-100 times more potent than morphine.
Geographical variation: Opioid overdose rates can vary across different states and regions within the United States. Some areas, particularly in the Midwest and Appalachia, have been heavily affected by the opioid crisis, experiencing higher rates of opioid overdose deaths.
Impact on demographic groups: Opioid overdoses have affected various demographic groups, but certain populations have been disproportionately impacted. Men, individuals aged 25-54, and non-Hispanic White individuals have experienced higher rates of opioid overdose deaths. However, opioid use and overdose affect people from all backgrounds and socioeconomic statuses.
Opioid use disorder prevalence: The number of individuals struggling with opioid use disorder is significant. In 2019, an estimated 10.1 million people aged 12 or older misused opioids in the United States.
Tips and recommendations to prevent opioid overdose
Here are some tips and recommendations regarding the risks of opioid overdose. It is logical that the advice on dosage prevention follows directly from the most common risk factors of opioid overdose. Basically, I borrowed them from the National Harm Reduction Coalition – no one wrote so simply, clearly, and intelligently about this topic as they did.
No Combining Drugs
- Use only one drug at a time or reduce the amount of each drug used.
- Avoid combining alcohol with heroin or pills, as this combination is extremely dangerous.
- If using both alcohol or pills and heroin, consume the heroin first to better gauge the level of intoxication. Alcohol and benzos impair judgment, making it harder to remember or be aware of the amount consumed.
- Have a trusted friend present who is aware of the drugs taken and can provide assistance in case of an emergency.
Consider the Tolerance
- Use smaller amounts of a drug when sick or after a period of abstinence, as tolerance may be lower.
- Exercise caution and start with smaller doses when using drugs after a period of abstinence.
- Consider doing a tester shot or gradually increase the dosage.
- Try using a different method, such as snorting instead of injecting.
Remember about Quality
- Test the strength of a drug before consuming the full amount.
- Try to purchase drugs from the same dealer consistently to gain a better understanding of their quality.
- Seek information from others who have obtained drugs from the same dealer.
- Familiarize yourself with the pills you are taking.
- Exercise caution when switching from one type of opioid pill to another.
No Using Alone
- Whenever possible, use drugs with a trusted friend present.
- Develop an overdose plan with friends or partners.
- Keep the door unlocked or slightly ajar for easier access in case of an emergency.
- Inform someone you trust about your drug use and request periodic check-ins.
- Some individuals may have a sense of when they are about to overdose. If you possess this ability, consider having naloxone (a medication used to reverse opioid overdoses) readily available. There have been cases where people have self-administered naloxone.
Take Care of Your Health
- Stay hydrated and maintain a balanced diet.
- If you have liver damage, avoid pharmaceuticals with high levels of acetaminophen, such as Vicodin and Percocet.
- Carry your inhaler if you have asthma and inform your friends about its location in case of breathing difficulties.
- Exercise caution when using drugs after a period of sickness, weight loss, or feeling weak, as it can impact your tolerance.
- Consult with a nonjudgmental doctor to assess other health factors that may increase your risk of stimulant overdose, such as high blood pressure, high cholesterol, heart disease, or other physical conditions that may raise the risk of a stroke or heart attack.
Other tips
- Follow the prescribed dosage and instructions.
- Seek medical advice before stopping or changing medication.
- Store opioids safely: Keep opioids securely stored in a locked cabinet or container to prevent accidental ingestion by children, adolescents, or visitors. Proper storage reduces the risk of unauthorized use or accidental overdose.
- Dispose of unused opioids properly: When you no longer need your opioid medication or it has expired, follow recommended disposal guidelines. Some communities have drug take-back programs or designated drop-off locations.
- Educate yourself and others: Stay informed about the risks associated with opioid use and overdose. Share this knowledge with friends, family, and community members to raise awareness and help prevent overdose incidents.
- Be prepared to respond to an overdose: Learn about naloxone, an opioid overdose-reversal medication, and how to administer it. Consider having naloxone on hand if you or someone you know is at risk of opioid overdose. Training on CPR and rescue breathing techniques can also be valuable in case of an emergency.
Conclusion

What is an opioid overdose? It’s not just a medical or personal problem. Opioid overdose poses a significant and ongoing risk, contributing to a public health crisis in many countries, including the United States. The situation demands attention and action from individuals, healthcare providers, policymakers, and communities. Understanding the risks associated with opioid use and overdose is crucial in addressing this complex issue. Here are key points to consider:
Opioid overdose deaths: Opioid overdose deaths have been on the rise, with opioids accounting for a substantial portion of all drug overdose deaths. Synthetic opioids, particularly illicitly manufactured fentanyl, have become a major concern.
Prescription practices: Proper prescribing practices, including risk assessment, judicious use of opioids, and considering alternative pain management options, are important for preventing misuse and overdose.
Substance use disorder: Opioid misuse and overdose often indicate an underlying substance use disorder. Providing accessible and comprehensive treatment options, including medication-assisted treatment, counseling, and support services, is critical in addressing the root causes of opioid addiction.
Harm reduction: Implementing harm reduction strategies such as naloxone distribution programs, safe injection sites, and education on safer drug use practices can save lives and reduce the negative consequences associated with opioid use.
Education and awareness: Raising public awareness about the risks of opioid use, signs of overdose, and available resources is crucial in preventing overdoses and promoting safer practices.
Collaboration and policy changes: Combating the opioid crisis requires a collaborative effort involving healthcare providers, policymakers, law enforcement, and community organizations. Implementing evidence-based policies, improving access to treatment, and addressing the social determinants of opioid addiction can help mitigate the crisis.
It is important for individuals to take precautions, such as following prescribed medication instructions, storing opioids safely, and being aware of potential interactions. Proper disposal of unused opioids and being prepared to respond to an overdose with naloxone and appropriate emergency procedures are also essential.
By addressing the risks associated with opioid use, increasing access to treatment, and implementing comprehensive prevention strategies, we can work towards reducing opioid overdose incidents and supporting individuals affected by opioid addiction.
✔️
This marks the finish of today’s session. It is my hope that this piece was enlightening.
If you want to advance the growth of this blog, I suggest the following actions:
- Subscribe to our social networks.
- Circulate a link to this article among your associates.
- Give recognition to this blog on relevant platforms or discussion groups.
Should you identify any necessary additions or corrections in this article, feel free to initiate a dialogue with me via Contact Form. I am always open to communication.
I appreciate your valuable time and consideration 👨⚕️




