Recently, I came across a relatively new and well-written article on the seemingly eternal topic of our reward system and addiction. A few hours later, I found myself deeply immersed in the latest research and publications by scientists on this topic. Below you will find a brief repetition of the basics and what new neuroscience has learned about addiction over the past year or two. Have fun reading.
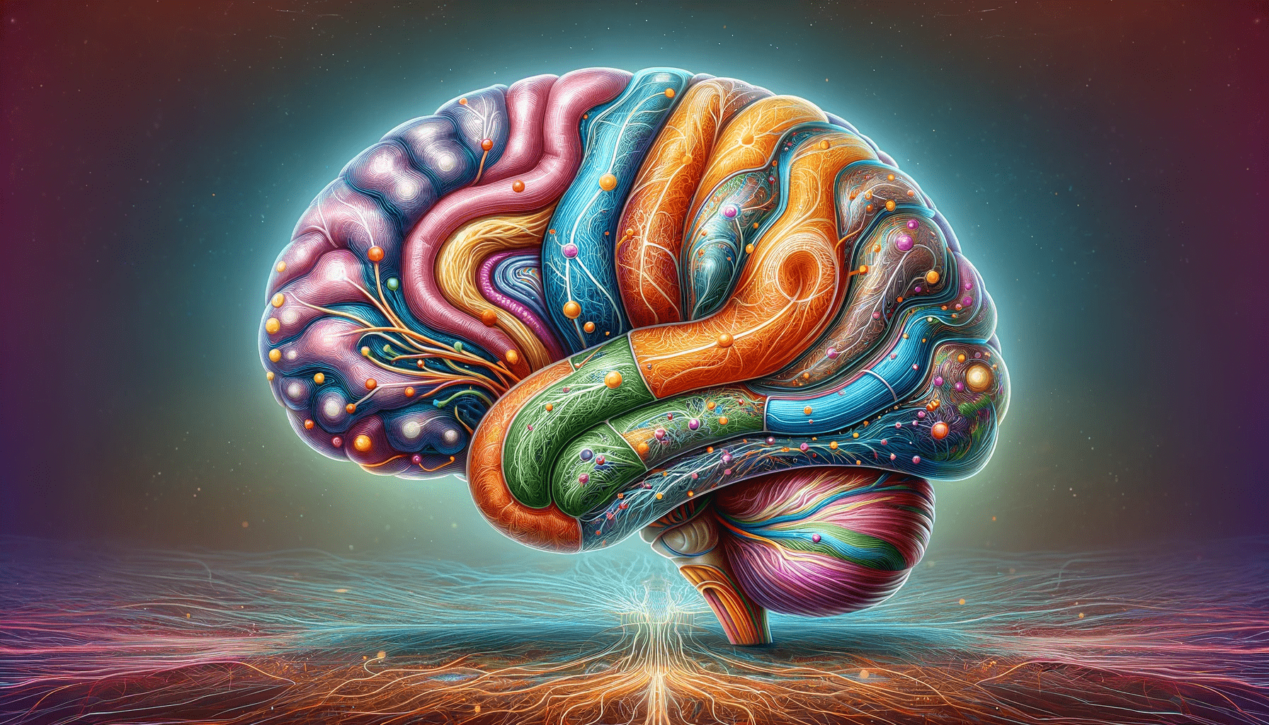
Brain’s Reward Circuit

Imagine a bustling city inside your brain, where messages are constantly sent and received. At the heart of this city lies the nucleus accumbens, a critical station in the brain’s reward system. Just like a city depends on its power grid, the brain relies on a neurotransmitter called dopamine. Whenever you experience something rewarding, like a delicious meal or a warm hug, dopamine travels to the nucleus accumbens, lighting up the brain’s reward circuit and making you feel good. This dopamine surge is what motivates us to seek out these pleasurable experiences again.
The Intruder: Drugs and Their Impact
Drugs, however, hijack this system. They increase dopamine levels in the nucleus accumbens, sometimes to levels much higher than natural rewards. This results in an intense feeling of euphoria. But drugs don’t just stop there. They also trigger changes in other areas of the brain like the prefrontal cortex, which is responsible for decision-making and impulse control, and the amygdala, which handles emotions. As a result, drug use can lead to impaired self-control and heightened emotional responses, making it even harder to resist the drug.
The Double-Edged Sword of Dopamine

Interestingly, not all drugs increase dopamine levels in the same way. Some act directly on dopamine neurons in the ventral tegmental area (VTA), a region that sends dopamine to the nucleus accumbens. Others work indirectly by affecting different neurotransmitters like opioids and cannabinoids, which also influence how we perceive pleasure and pain.
The Ripple Effect: How Addiction Reshapes the Brain
Repeated use of drugs leads to neuroadaptations – changes in how neurons communicate with each other. These changes occur in multiple neurotransmitter systems, including the glutamatergic system that enhances neuron excitability and the GABAergic system that inhibits action potential transmission. The opioid, endocannabinoid, cholinergic, serotonin, and noradrenergic systems also change, altering how we process emotions and pleasure.
Conditioning: The Brain’s Learning Trap
With continued drug use, a person’s brain starts to associate the drug with its environment, including places, people, or even emotional states. This is called conditioning. The dopamine neurons begin to fire in anticipation of the drug, even before it’s taken. This process is similar to how we learn other behaviors, involving changes in synaptic strength and neuronal communication patterns.
The Diminishing Returns of Addiction
A paradox arises in addiction. While the brain becomes more sensitive to the anticipation of drug use, its response to the actual consumption of the drug diminishes. This reduced sensitivity also extends to natural rewards like food or social interactions, making them less appealing. This change is partly due to decreased dopamine receptor expression in the brain’s reward regions. The complexities of these changes, including inconsistencies in research findings, highlight the dynamic and state-dependent nature of dopamine as a neuromodulator.
Recent Neuroscience Discoveries

- Cerebellum and Basal Ganglia Connection: New research has established a direct pathway between the cerebellum and the basal ganglia, linking these two brain regions in reward processing and addiction. The cerebellum, traditionally associated with motor learning, is now understood to influence dopamine levels in the basal ganglia, a key area in reward-based learning and decision-making. This discovery opens new avenues for understanding addiction and potentially for developing treatments for neurodegenerative diseases like Parkinson’s.
- Altered Reward Perception in Cocaine Addiction: Studies have shown that cocaine addiction alters the perception of reward, but not the expectation of it. In people with chronic cocaine addiction, there is a marked reduction in how their reward system responds to the outcomes of decisions. This means that the brain’s ability to signal when an unexpected reward is received is weakened, making it difficult for individuals to learn from experience and modify decision-making for better outcomes. This could inform therapeutic strategies targeting addictive behaviors.
- Impact of Socioeconomic Status on Reward Sensitivity: A study from MIT has found that the brain’s response to reward is linked to socioeconomic background. Adolescents from lower socioeconomic statuses showed less activation in the striatum during reward-related tasks, indicating a dampened response to reward. This finding suggests that reward sensitivity in the brain can be shaped by the environment and has far-reaching implications for understanding the development of addiction in different socioeconomic contexts.
- Whole-Brain Tracking of Reward Processing: Advanced techniques are now used to map the brain’s response to rewards at a whole-brain level. This approach has enabled researchers to identify how different brain regions are activated in response to natural and addictive rewards (like cocaine and sugar), providing a comprehensive view of the neural circuits involved in reward processing and addiction. This method can also help in understanding synaptic changes like the increase in silent synapses and alterations in NMDAR-mediated currents, which are crucial in addictology.
- Reward-Based Treatment for Addiction: There is growing interest in reward-based treatments for addiction, like contingency management. This approach rewards individuals for not engaging in addictive behaviors, offering incentives like prizes or gift cards. This method is based on the principle that rewarding positive behavior can help rebalance the reward pathway in the brain, which drugs hijack. Contingency management has shown effectiveness in promoting abstinence from various substances, including cocaine, methamphetamine, tobacco, alcohol, opioids, cannabis, and benzodiazepines.
Key Takeaways
These new findings add depth to our understanding of addiction and the reward system. They suggest that:
- Addiction exploits the brain’s natural reward system, leading to an overpowering urge to seek drugs. But the brain’s reward circuitry is not just confined to traditional areas like the nucleus accumbens but involves more extensive brain networks, including the cerebellum.
- Neuroadaptations in the brain decrease the ability to resist drugs and reduce sensitivity to natural rewards. The alteration in reward perception, particularly in cocaine addiction, highlights the complex interplay between expectation and experience in addictive behaviors.
- Dysregulation in reward learning underscores the challenges in treating addiction and points toward potential new treatment avenues. The brain’s conditioning to drugs complicates addiction, making recovery a challenging but achievable journey.
- Reward-based treatments like contingency management offer promising alternatives to traditional addiction therapies by leveraging the brain’s inherent reward system.
Incorporating these insights into our understanding of addiction enriches the narrative around how addictive behaviors are formed and maintained, and importantly, how they can be effectively treated. This evolving landscape of knowledge continues to offer hope and direction in addressing the challenges of addiction.
In conclusion, the brain’s reward system, when influenced by addiction, shows us the incredible adaptability of our brain, but also its vulnerability. Understanding these mechanisms is not only fascinating from a scientific perspective but also crucial in developing effective treatments and interventions.
Find More
- The Neuroscience of Drug Reward and Addiction
- The cerebellum directly modulates the substantia nigra dopaminergic activity
- Reduced neural encoding of utility prediction errors in cocaine addiction
- How the brain responds to reward is linked to socioeconomic background
- Contingency Management Is a Powerful Clinical Tool for Treating Substance Use



This was beautiful! Thank you for your reflections.
Ive read several. Just right stuff here! Certainly price bookmarking for revisiting. I wonder how a lot effort you place to create this kind of great informative website