Addiction stands as a multifaceted challenge that straddles the domains of psychology and physiology, presenting a complex interplay of brain mechanisms, emotional responses, and social factors. At its core, addiction encompasses a range of behaviors and dependencies, from substance abuse to compulsive engagements in activities like gambling, eating, or internet use. This complexity arises from the brain’s reward system being hijacked, leading to a cycle of cravings, indulgence, and reinforcement despite adverse consequences. The psychological aspect is equally intricate, often rooted in attempts to cope with stress, trauma, or underlying mental health disorders. This dual nature of addiction underscores the critical need for interventions that address both the mind and body.
Enter Cognitive-Behavioral Therapy (CBT), a therapeutic approach that has gained prominence for its effectiveness in treating a wide array of psychological states, including addiction. CBT operates on the premise that maladaptive thoughts and beliefs contribute to negative emotions and behaviors, including those associated with substance use and addictive behaviors. By identifying and challenging these cognitive distortions, and by developing healthier coping mechanisms, CBT equips individuals with the tools to manage their addiction and mitigate its impact on their lives. This approach not only addresses the immediate behaviors associated with addiction but also targets the underlying cognitive processes, making it a potent intervention for those seeking to overcome the grips of substance use and behavioral addictions.
Understanding Addiction
I don’t think I’ll get tired of writing about it, and I hope you won’t get tired of reading.
Addiction represents a spectrum of conditions characterized by the compulsive engagement in rewarding stimuli, despite detrimental consequences. It manifests most prominently through substance use disorders and behavioral addictions, such as gambling, eating, or internet use. This section elucidates the gradations of substance interaction—use, abuse, and addiction—while exploring the psychological, neurobiological, and socio-environmental facets contributing to addiction.
Substance Use vs. Abuse vs. Addiction
- Substance Use involves the consumption of drugs or alcohol at levels or in ways that don’t interfere with health, social, or occupational responsibilities. It’s characterized by control over the use of substances and absence of negative consequences.
- Substance Abuse marks a transition from use to more risky behaviors. It’s defined by the recurrent use of substances in ways that cause significant impairment, such as health problems, disability, and failure to meet responsibilities at work, school, or home.
- Addiction is the most severe form of substance engagement. It’s characterized by the inability to stop using the substance despite adverse health, social, and legal consequences. Addiction involves physical or psychological dependency, with increased tolerance and withdrawal symptoms upon cessation.
Psychological and Neurobiological Underpinnings
Addiction disrupts the brain’s natural reward system, primarily through the neurotransmitter dopamine. The brain registers all pleasures in the same way, whether they originate from a psychoactive substance, a monetary reward, a social interaction, or a satisfying meal. In an addict’s brain, dopamine pathways are hijacked by the substance or behavior, leading to the reinforcement of unhealthy behaviors while neglecting natural rewards.
The psychological aspects of addiction encompass a range of emotional and cognitive processes, including:
- Cravings: Intense desires or urges for the substance or behavior.
- Compulsion: A psychological push towards substance use or behavior despite understanding its harmful effects.
- Cognitive distortions: Misguided thoughts and beliefs that rationalize substance use or addictive behaviors.
Environmental, Genetic, and Personal Factors
- Environmental Factors: Include the availability of substances, social pressure, and exposure to stress or trauma. Environments that foster substance use or provide consistent exposure to addictive behaviors increase the risk of developing addictions.
- Genetic Factors: Genetics play a significant role, contributing to about half of the individual’s risk of addiction. Family history of addiction increases susceptibility, indicating the interplay between genetic predisposition and environmental exposure.
- Personal Factors: Personal characteristics such as age, gender, and the presence of other mental health disorders can influence addiction vulnerability. Early exposure to substances or traumatic experiences can also heighten the risk.
The Basics of Cognitive-Behavioral Therapy
Cognitive-Behavioral Therapy (CBT) is a widely recognized and empirically supported psychological treatment that has evolved significantly since its inception. Its development is attributed to the pioneering work of Dr. Aaron T. Beck in the 1960s, who initially applied it to depression. Beck observed that patients often held negative beliefs about themselves, the world, and the future, which affected their emotions and behaviors. Over the years, CBT has expanded its application to a variety of psychological disorders, including anxiety, PTSD, OCD, and notably, addiction.
Historical Background and Development
The roots of CBT lie in the confluence of behavioral and cognitive theories, acknowledging that psychological distress is often a result of maladaptive thoughts and behaviors. This therapy emerged as a response to the limitations of psychoanalytic and behaviorist approaches, offering a more comprehensive model that considers thoughts, emotions, and behaviors as interconnected. Its foundation rests on the principle that changing maladaptive thought patterns can lead to changes in behavior and emotional state.
Core Principles of CBT
The core principles of CBT revolve around the interconnectedness of thoughts, feelings, and behaviors. CBT posits that:
- Thoughts Influence Feelings and Behaviors: Negative and unrealistic thoughts can lead to distressing emotions and dysfunctional behaviors.
- Feelings Influence Thoughts and Behaviors: Emotional responses can influence our thought patterns and reactions in certain situations.
- Behaviors Influence Thoughts and Feelings: Changing one’s behavior can affect the way we think and feel about a situation.
By understanding these interconnections, individuals can identify and modify their patterns of thinking, feeling, and behaving to cope with psychological distress.
The Process of CBT
- Identification of Problematic Behaviors and Thought Patterns: The initial step involves collaboratively working with the therapist to identify specific challenges and maladaptive patterns affecting the individual’s life. This may involve self-monitoring to become more aware of these patterns.
- Development of Strategies to Address Them: Through a variety of techniques, such as cognitive restructuring, individuals learn to challenge and change unhealthy thoughts and beliefs. This might involve examining the evidence for and against certain beliefs, exploring alternative perspectives, and testing these beliefs in real-world situations.
- Implementation of Coping Mechanisms: CBT equips individuals with practical skills to manage stressful situations and emotional distress. Coping strategies might include problem-solving, assertiveness training, relaxation techniques, and mindfulness practices. These skills are practiced within and outside of therapy sessions to build competence and confidence.
The process of CBT is highly collaborative, with the therapist and client working together to set goals, identify challenges, and develop strategies. This empowering approach fosters a sense of agency in individuals, encouraging them to take active roles in their treatment and recovery. Through CBT, individuals learn not only to address current issues but also to apply these skills to future challenges, promoting long-term mental health and resilience.
CBT in the Context of Addiction Treatment

Cognitive-Behavioral Therapy (CBT) has been effectively adapted to address the unique challenges of addiction treatment. Its flexibility and focus on the interplay between thoughts, emotions, and behaviors make it particularly suitable for helping individuals overcome addiction.
CBT for addiction involves several tailored strategies to meet the specific needs of individuals struggling with substance use disorders or behavioral addictions:
- Addressing Cravings and Triggers: CBT helps individuals identify specific cues (triggers) that lead to substance use or addictive behaviors. These triggers can be external, such as places or people, or internal, such as emotions or thoughts. Once identified, CBT teaches coping strategies to manage cravings and reduce the likelihood of substance use when encountering these triggers.
- Relapse Prevention: An integral part of CBT in addiction treatment is preparing individuals for potential relapse scenarios. This involves recognizing early warning signs, developing a plan to cope with high-risk situations, and learning to view relapse as a temporary setback rather than a failure. This perspective helps in maintaining progress and returning to sobriety more quickly.
Role of CBT in Modifying Cognitive Distortions
Cognitive distortions are inaccurate thoughts that reinforce negative thinking and behavior patterns. In the context of addiction, these might include beliefs like “I can’t cope with stress without substances,” or “I’m not strong enough to resist cravings.” CBT aims to identify and challenge these distortions through:
- Cognitive Restructuring: A technique used to challenge and change irrational thoughts. Individuals learn to recognize their cognitive distortions, analyze them in light of evidence, and reframe them into more balanced and realistic thoughts.
- Enhancing Self-Efficacy: Building the belief in one’s ability to resist substance use and cope with challenges without relying on addictive behaviors.
CBT and Harm Reduction
Cognitive-Behavioral Therapy (CBT) and harm reduction represent complementary approaches in the realm of addiction treatment. While CBT focuses on modifying maladaptive thought patterns and behaviors, harm reduction emphasizes minimizing the negative consequences of substance use without necessarily requiring abstinence. Together, they offer a pragmatic and compassionate framework for addressing addiction.
CBT enhances harm reduction efforts by providing individuals with cognitive and behavioral tools to reduce risky behaviors and mitigate harm. Key aspects include:
- Skill Development: CBT teaches coping skills for dealing with cravings, emotional distress, and social pressure, which can reduce reliance on substances as a means of coping.
- Behavioral Change: By addressing the underlying thought patterns that contribute to substance use, CBT helps individuals make informed decisions about their drug use, potentially leading to reduced consumption or safer use practices.
- Emotional Regulation: CBT strategies improve emotional awareness and regulation, aiding individuals in managing the emotional and psychological triggers that may lead to risky substance use behaviors.
CBT + Harm Reduction = Comprehensive Addiction Treatment
Integrating CBT with harm reduction strategies creates a synergistic effect in addiction treatment, offering a more holistic and flexible approach. This integration supports individuals at various stages of readiness for change by:
- Providing a Continuum of Care: From those not ready to cease substance use to those aiming for abstinence, CBT combined with harm reduction addresses the diverse needs and goals of individuals.
- Empowering Choice: Encouraging personal agency and informed decision-making regarding substance use and health behaviors.
- Enhancing Engagement: Reducing the stigma associated with substance use and treatment, thereby increasing the likelihood of individuals seeking and staying in treatment.
Incorporating CBT into harm reduction-based treatment plans acknowledges the complexity of addiction and respects the individual’s autonomy and capacity for change. It recognizes that the journey towards recovery is personal and varied, requiring a range of strategies to support health and well-being. Through this comprehensive approach, individuals are better equipped to navigate the challenges of addiction, improve their quality of life, and move towards healthier outcomes at their own pace.
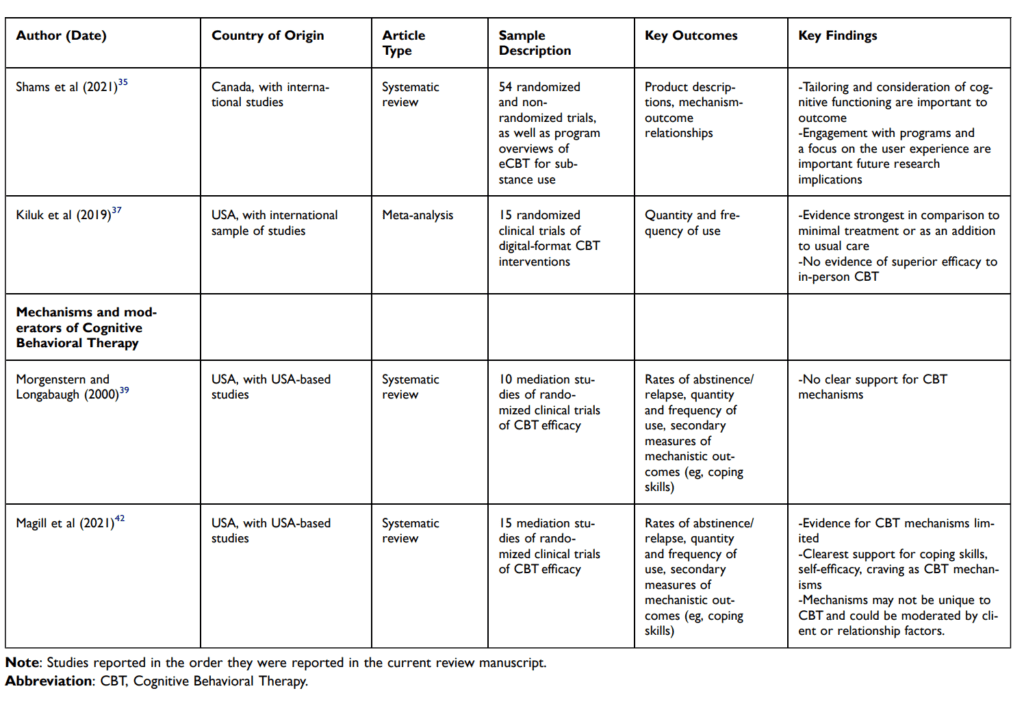
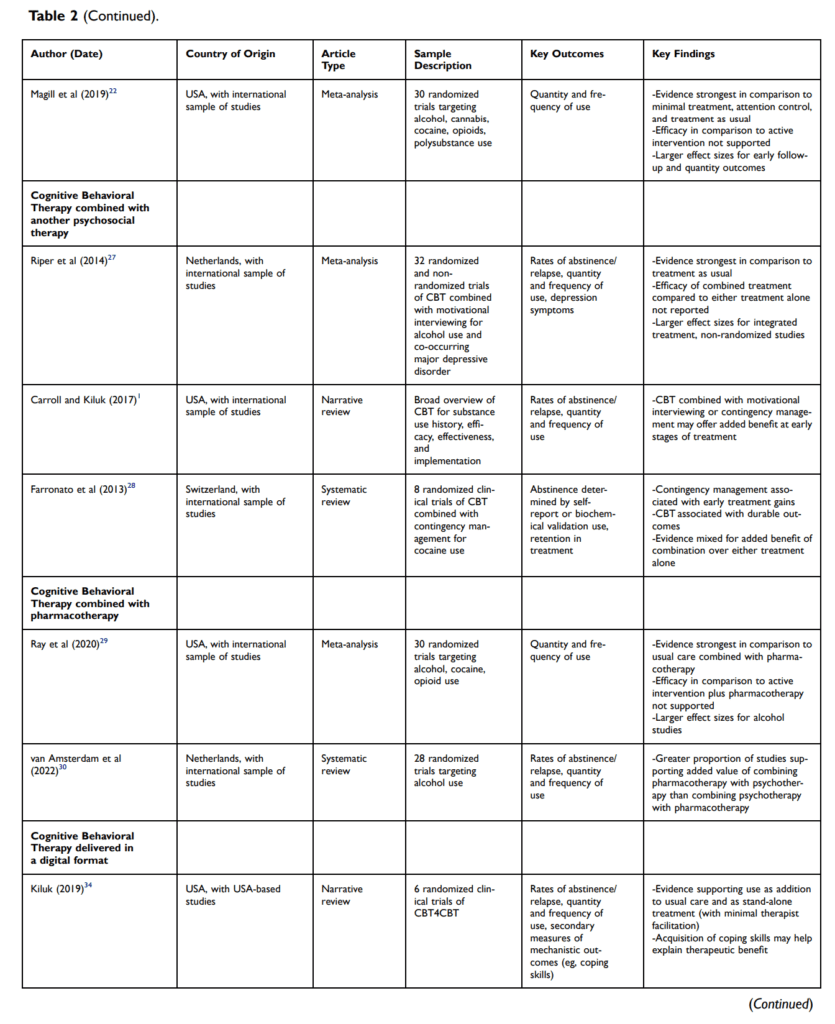
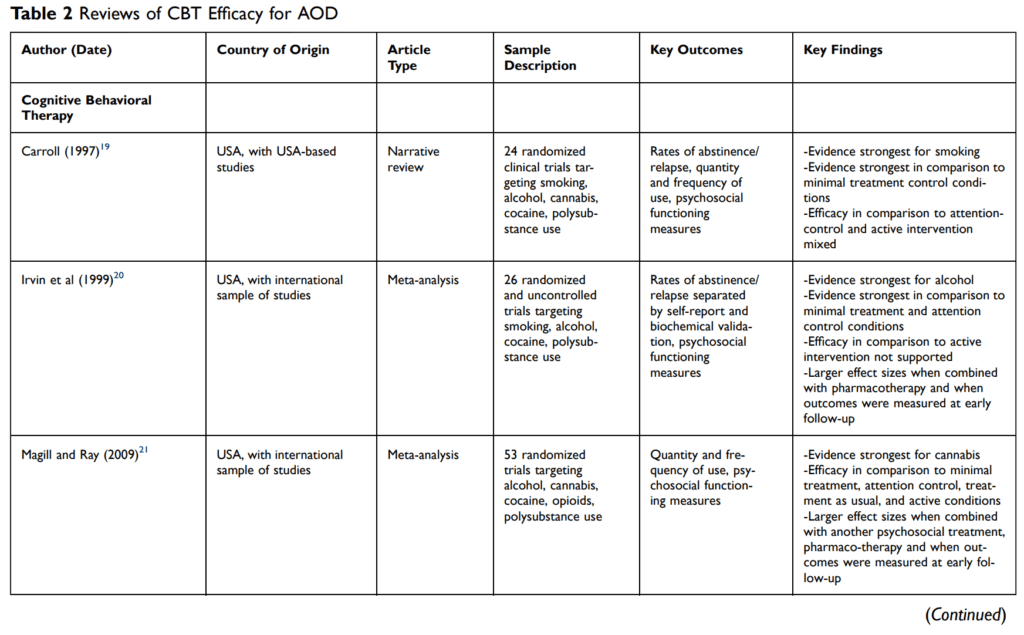
The Effectiveness of CBT Towards Addiction
Here it was possible to break up the conversation into a separate article, but I will limit myself to tables from a recent study that analyzed the effectiveness of the approach we are considering in different conditions, scenarios and application points.
Challenges and Considerations in Applying CBT to Addiction Treatment
While CBT is a powerful tool in addiction treatment, its application comes with certain limitations and challenges. Understanding these hurdles is crucial for optimizing the effectiveness of CBT in diverse populations and individual circumstances.
Limitations and Challenges
- Variability in Response: Not everyone responds to CBT in the same way. Factors such as the nature and severity of the addiction, co-occurring mental health disorders, and individual motivation levels can affect outcomes.
- Therapeutic Engagement: Successful CBT requires active participation and homework compliance from the patient, which can be challenging for some, especially those with severe addiction or low motivation.
- Accessibility and Resources: There may be barriers to accessing quality CBT, including financial constraints, lack of trained therapists, and geographical limitations.
- Relapse Rates: While CBT aims to equip individuals with skills to manage cravings and triggers, relapse remains a reality for many, necessitating ongoing support and possibly multiple treatment attempts.
Importance of Individualized Treatment Plans
Recognizing the uniqueness of each individual’s journey through addiction and recovery is paramount. An individualized treatment plan, tailored to the specific needs, goals, and circumstances of the person, is more likely to be effective. Such customization should consider:
- The specific substance(s) used and patterns of use.
- Co-occurring mental health conditions and how they interact with addiction.
- Personal motivations for recovery, readiness for change, and personal strengths.
- Cultural, social, and environmental factors influencing the individual’s life and recovery.
Support Systems, Healthcare Professionals, and Continuous Care
The effectiveness of CBT in addiction treatment is significantly enhanced by the presence of a strong support system, the expertise of healthcare professionals, and a commitment to continuous care.
- Support Systems: Family, friends, and peer support groups can provide emotional encouragement, accountability, and practical assistance throughout the recovery process. Engaging with communities, such as 12-step programs or recovery-focused online forums, can offer additional layers of support and understanding.
- Healthcare Professionals: The expertise of trained therapists, addiction specialists, and mental health professionals is crucial in delivering effective CBT. Their guidance helps individuals navigate the challenges of recovery, adjust treatment plans as needed, and address any co-occurring mental health issues.
- Continuous Care: Addiction is often a chronic condition requiring ongoing management. Continuous care may include regular therapy sessions, booster sessions post-treatment, and check-ins to prevent or address relapse. This long-term perspective acknowledges recovery as a dynamic and evolving process.
Addressing these challenges and considerations necessitates a comprehensive and flexible approach to addiction treatment. By tailoring CBT to the individual, leveraging support systems, and ensuring access to skilled healthcare professionals and continuous care, the potential of CBT to facilitate meaningful and sustained recovery can be maximized.
Future Directions in CBT for Addiction Treatment
Research into CBT for addiction is expanding into new areas, exploring its efficacy across a broader spectrum of substances and behaviors, and delving into the mechanisms that underpin its success. Current trends include:
- Precision Medicine: Tailoring CBT interventions to individual genetic, environmental, and psychological profiles to enhance treatment efficacy.
- Combination Therapies: Investigating the synergy between CBT and other therapeutic approaches, including pharmacotherapy, to address complex cases of addiction.
- Longitudinal Studies: Focusing on the long-term outcomes of CBT for addiction to identify factors that contribute to sustained recovery and those that predict relapse.
- Teletherapy: Remote CBT sessions via video conferencing have become more common, breaking down geographical and logistical barriers to treatment.
- Virtual Reality (VR) and Gamification: Emerging technologies like VR are being explored for their potential to simulate real-life situations that can trigger substance use, allowing individuals to practice coping strategies in a safe, controlled environment.
- Mobile Apps and Digital Platforms: Apps designed to support CBT practices enable users to track moods, thoughts, and behaviors, access coping strategies, and even receive guidance through AI-driven chatbots.
The Evolving Landscape of Addiction Treatment
The future of addiction treatment, with CBT at its core, is moving towards more holistic and integrated approaches that address the entirety of an individual’s experience:
- Holistic Health Focus: Recognizing the importance of addressing physical health, mental health, and social well-being in conjunction, rather than focusing solely on ceasing substance use.
- Personalized Care Plans: Leveraging data analytics and AI to create highly personalized treatment plans that evolve in real-time based on an individual’s progress and changing needs.
- Integration of Harm Reduction: Combining CBT with harm reduction strategies more systematically to provide a spectrum of options that cater to individuals at different stages of readiness for change.
As research continues to unfold and technology advances, the application of CBT in addiction treatment is set to become more effective, personalized, and accessible. These future directions not only promise to enhance the quality of care for individuals battling addiction but also offer hope for more successful recovery outcomes, contributing to a broader understanding and acceptance of addiction as a treatable condition.
Conclusion
Throughout this exploration of Cognitive-Behavioral Therapy for addiction and harm reduction, we’ve delved into the multifaceted nature of addiction, the foundational principles of CBT, and its practical application in treating addictive behaviors. We’ve also discussed the synergistic relationship between CBT and harm reduction strategies, the challenges and considerations in implementing CBT, and looked ahead to the future directions of this therapeutic approach.
CBT stands out as a potent, evidence-based tool in the arsenal against addiction. By equipping individuals with practical strategies for managing cravings, avoiding triggers, and preventing relapse, CBT empowers those struggling with addiction to take significant steps towards recovery.
The integration of CBT with harm reduction principles further enhances its applicability and effectiveness, acknowledging the spectrum of goals and readiness levels among individuals facing addiction. This approach respects the individual’s journey, promoting safer practices and gradual changes that lead to improved health and well-being.
However, the successful application of CBT in addiction treatment is not without its challenges. It requires individualized treatment plans, the support of healthcare professionals, and the active involvement of the individual in their therapeutic journey. Continuous care and support systems play crucial roles in sustaining the gains made through therapy.
In conclusion, Cognitive-Behavioral Therapy offers significant promise as a transformative tool in the fight against addiction. Its ability to address the complex interplay of thoughts, emotions, and behaviors that underpin addictive patterns positions CBT as a cornerstone of effective addiction treatment and harm reduction strategies. We encourage individuals grappling with addiction and healthcare professionals alike to consider the benefits of CBT. By adopting a holistic approach that includes CBT, we can move closer to overcoming the challenges of addiction, fostering a path toward healing, recovery, and a more hopeful future.
Find More
- Efficacy of Cognitive Behavioral Therapy for Alcohol and Other Drug Use Disorders.
- Combined Pharmacotherapy and Cognitive Behavioral Therapy for Adults With Alcohol or Substance Use Disorders: A Systematic Review and Meta-analysis
- When neurostimulation joins cognitive-behavioral therapy. On the need of combining evidence-based treatments for addiction disorders




