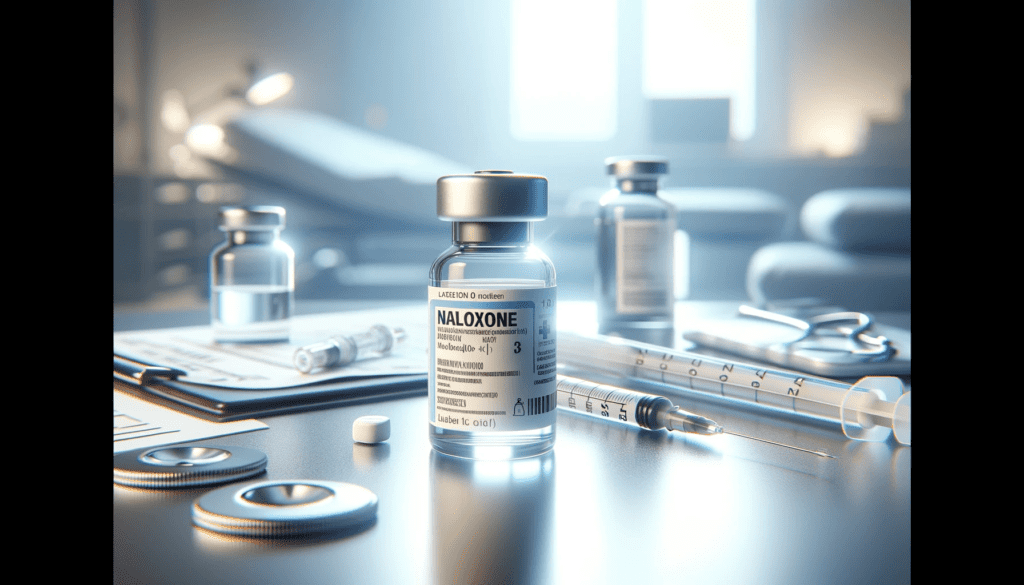
Naloxone is a critical medication in both emergency medicine, harm reduction, and addiction treatment, particularly in the context of opioid overdoses. Here’s a comprehensive overview of its role and importance:
Naloxone, also known by its brand name Narcan among others, is an opioid antagonist. This means it binds to opioid receptors in the brain but, unlike opioid agonists (like morphine, heroin, or fentanyl), it does not activate these receptors. Instead, it blocks and reverses the effects of other opioids. This action is crucial in counteracting life-threatening depression of the central nervous system and respiratory system caused by opioid overdose.
Main Purposes of Using Naloxone
Opioid Overdose Reversal: Naloxone is most commonly used to counteract life-threatening depression of the central nervous system and respiratory system caused by opioid overdose. This includes overdoses from prescription opioids (like oxycodone or morphine), heroin, and synthetic opioids (like fentanyl).
Harm Reduction Programs: Individuals who use opioids or their family members are given naloxone kits. They are trained to use naloxone in case of an overdose, providing a crucial window for emergency services to arrive. Given its importance in treating opioid overdoses, naloxone is often made available to emergency responders, harm reduction sites, and, in some regions, over the counter to the general public.
Diagnostic Tool: In a hospital setting, naloxone can be used diagnostically to determine whether a person’s symptoms (such as unconsciousness) are due to an overdose of opioids.
Postoperative Care: A patient recovering from surgery has been given opioid painkillers and shows signs of respiratory depression. Naloxone may be administered to counteract the effects of opioids, ensuring safe recovery.
Chronic Pain Management: Patients on high doses of opioids for chronic pain management may have naloxone on hand as a precaution. In case of accidental overdose due to medication error or sensitivity, naloxone can be used for immediate reversal.
History of Naloxone

Naloxone has an interesting history marked by critical milestones in its development and implementation.
Early Development
Naloxone was first synthesized in 1961 by Mozes J. Lewenstein and Jack Fishman, two researchers at the company Sankyo in Japan. Their work was part of a broader effort to create opioid antagonists.
The patent for naloxone was acquired by Endo Laboratories, a small pharmaceutical company in New York. Initial studies focused on its potential to reverse opioid overdose.
FDA Approval and Early Use
Naloxone was approved by the U.S. Food and Drug Administration (FDA) in 1971 for the treatment of opioid overdose. Initially, naloxone was primarily used in medical settings, especially emergency rooms, to treat acute opioid overdose. It was administered intravenously by healthcare professionals.
Expansion of Use and Public Access
With the escalation of the opioid crisis in the 1990s and 2000s, largely fueled by the widespread prescription of opioid pain relievers and the subsequent rise in heroin use, naloxone’s importance grew.
Naloxone became a cornerstone of harm reduction strategies. Programs began distributing naloxone to people who use opioids, as well as their friends and families, to use in emergencies.
Laws and regulations in many areas were amended to increase access to naloxone. These changes often included Good Samaritan laws to protect those administering naloxone in an emergency.
Innovations in Administration
In 2015, the FDA approved a nasal spray version of naloxone, making it easier for non-medical personnel to administer.
Auto-injectors, similar to epinephrine pens for allergic reactions, were also developed, providing another user-friendly option for naloxone administration.
Recent Developments
Naloxone has become increasingly available over-the-counter in many places, and it’s regularly carried by first responders, including police and emergency medical technicians.
There have been significant efforts in public health campaigns to raise awareness about opioid overdose and the availability of naloxone, including training on its use.
Research continues into improving naloxone formulations and delivery methods, as well as integrating its use into broader strategies for addressing the opioid crisis.
Chemical Structure of Naloxone
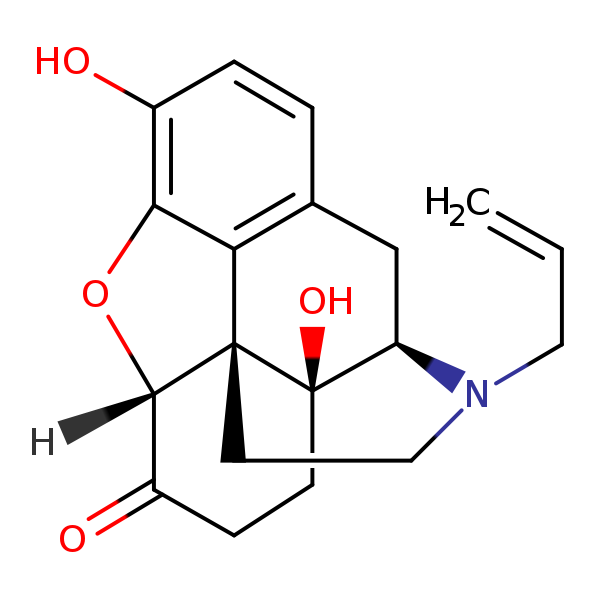
Naloxone’s molecular formula is C19H21NO4. It features a morphinan skeleton, which is common in many opioid compounds. This structure comprises a fused ring system, including a benzene ring (aromatic ring), a cyclohexene ring, and two cyclohexane rings.
An allyl group (CH2=CH-CH2-) is attached to the nitrogen atom. This is crucial for its antagonist properties.
A ketone group (C=O) is located on the cyclohexenone ring.
An alcohol group (hydroxyl, -OH) on the cyclohexane ring.
An ether linkage (–O–) connects the phenolic ring to the rest of the structure.
Naloxone has several chiral centers, which means it can exist in various stereoisomeric forms. However, the clinically used naloxone is a specific isomer.
Comparison with Similar Compounds
Naltrexone shares a very similar structure to naloxone, with the primary difference being the substitution of the allyl group on naloxone with a cyclopropylmethyl group in naltrexone. This slight modification gives naltrexone a longer duration of action and makes it suitable for the treatment of alcohol and opioid dependence in a longer-term setting, as opposed to the emergency treatment of overdose.
Morphine, an opioid agonist, also shares the morphinan skeleton. Morphine has different functional groups, including two hydroxyl groups and a methyl ether, which contribute to its opioid agonist properties, as opposed to naloxone’s antagonist properties.
Fentanyl, a potent synthetic opioid agonist, does not share the morphinan structure but does interact with the same opioid receptors. Fentanyl’s structure is based on a phenethylamine core, which is significantly different from naloxone’s morphinan base.
Naloxone’s chemical structure is specifically tailored to bind to opioid receptors without activating them, thereby reversing the effects of opioid agonists. Its structural similarity to other opioid-related compounds, like naltrexone, is what allows it to effectively compete with and displace these agonists at the receptor sites. This precise molecular design underlines its effectiveness as an opioid antagonist, crucial in the management of opioid overdose.
Mechanism of Action of Naloxone
Naloxone’s mechanism of action is centered on its interaction with the opioid receptors in the central nervous system (CNS). This interaction is key to its ability to reverse the effects of opioids, particularly in overdose situations. Let’s delve into the details:
Binding to Opioid Receptors
Competitive Antagonism: Naloxone functions as a competitive antagonist at opioid receptors, with the highest affinity for mu-opioid receptors, which are predominantly responsible for the effects of opioids like analgesia (pain relief) and respiratory depression.
Displacement of Opioids: It competes with and displaces opioid agonists (substances that activate receptors) at these receptor sites. Due to its strong affinity, naloxone can effectively dislodge opioids even at low doses, reversing their effects.
Receptor Activity and Effects
Blocking Receptor Activation: Upon binding to the opioid receptors, naloxone prevents the activation of these receptors by opioid agonists. It doesn’t elicit any intrinsic activity at the receptor, meaning it doesn’t activate the receptor’s typical response.
Reversal of CNS and Respiratory Depression: By blocking opioid receptor activity, naloxone reverses central nervous system and respiratory depression – the most life-threatening aspects of opioid overdose. This action restores normal respiratory function and consciousness in individuals experiencing an overdose.
Rapid Onset and Duration of Action
Quick Action: Naloxone acts quickly, typically showing effects within minutes of administration. This rapid onset is crucial in acute overdose situations where immediate reversal of respiratory depression is necessary.
Short Duration: It is a short-acting antagonist. Its effects generally last for about 30 to 90 minutes, depending on factors like the mode of administration and individual metabolism. This duration is often shorter than that of many opioids, necessitating careful monitoring and potentially repeated dosing in an overdose situation.
Impact on Different Opioid Receptors
Mu-Opioid Receptors: As mentioned, naloxone has the highest affinity for mu-opioid receptors. These receptors are primarily implicated in opioid-induced respiratory depression, analgesia, and euphoria.
Kappa and Delta Receptors: Naloxone also binds to kappa and delta opioid receptors, but its clinical effects are predominantly due to its action on mu receptors.
Non-Selective Antagonism: Naloxone’s non-selective antagonism across different opioid receptors makes it effective against overdoses from a broad spectrum of opioids.
Safety Profile: It’s considered a safe medication, even at high doses, with few side effects if given to a person who has not taken opioids.
Naloxone’s Duration of Action
Duration particularly relevant in the context of opioid overdose treatment, is influenced by several factors. Understanding these factors is crucial for effective clinical application.
- Typical Duration: Naloxone’s effects typically last between 30 minutes to an hour, though this can vary. It’s a relatively short-acting drug.
- Half-Life: The half-life of naloxone, which is the time it takes for half of the drug to be metabolized and eliminated from the body, is about 1 to 1.5 hours.
Factors Influencing Duration of Action
- Mode of Administration and Dosage
- Intravenous (IV): When administered intravenously, naloxone acts almost immediately but also has the shortest duration of action.
- Intramuscular (IM) or Subcutaneous (SC): These routes lead to a slightly slower onset but a longer duration of action.
- Intranasal (IN): This method is comparable to IM or SC in terms of onset and duration.
- Higher doses may have a longer duration of action, but this can vary based on individual metabolism and other factors.
2. Metabolism and Individual Factors:
- Liver Function: Naloxone is metabolized in the liver. Impaired liver function can slow its metabolism, potentially extending its duration of action.
- Renal Function: Since naloxone and its metabolites are excreted primarily by the kidneys, renal impairment might also affect its duration.
- Age, Body Weight, and Genetics: These can all affect how naloxone is metabolized and thus its duration of action.
- Concurrent Drug Use: The presence of other substances, especially other opioids or medications that affect liver enzymes, can influence how long naloxone works.
3. The Potency and Amount of Opioid Overdosed On: In cases of overdose with potent opioids like fentanyl, naloxone’s effect might be shorter than the duration of action of the opioid, necessitating repeated dosing.
Dosages, Routes, and Rules for Naloxone Use
Dosing
- The typical initial dose of naloxone for adults and children is 0.4 to 2 mg.
- This dosage can be repeated every 2 to 3 minutes if the desired response (restored breathing, consciousness) is not achieved.
- The total dose varies depending on the severity of the opioid overdose and the individual’s response.
High-Potency Opioid Overdose: Overdoses involving potent opioids like fentanyl may require higher initial doses, potentially in the range of 2 to 4 mg due to the stronger binding of these opioids to receptors.
Dosage Adjustments: Dosage may be adjusted based on factors like age, body weight, the opioid involved, and the individual’s health status.
Routes of Administration
Intravenous (IV):
- Fastest onset of action, typically within 1-2 minutes.
- Requires medical expertise for administration.
- Often used in hospital settings.
Intramuscular (IM) or Subcutaneous (SC):
- Easier to administer than IV, suitable for emergency responders and in community settings.
- Onset of action is usually within 3-5 minutes.
- Commonly used in pre-filled syringes or auto-injectors (e.g., Evzio).
Intranasal (IN):
- Nasal spray forms (e.g., Narcan, Nyxoid) offer ease of use without the need for injection.
- Onset is slightly slower than IM/IV but still rapid, typically within 3-5 minutes.
- Ideal for bystander administration in emergencies.
Rules of Use
Assessment Before Administration: Confirm signs of opioid overdose: unresponsiveness, shallow or absent breathing, and pinpoint pupils.
Ensure emergency medical services (EMS) are called as naloxone is not a substitute for medical care.
Post-Administration Monitoring: Monitor the individual’s breathing and consciousness after administration.
Be prepared to administer additional doses if the person doesn’t respond or if symptoms return, as naloxone’s duration of action can be shorter than that of the opioid.
Rescue Breathing/CPR: If trained, provide rescue breathing or CPR as needed while waiting for naloxone to take effect or if naloxone is not immediately effective.
Care After Reversal: Once the individual regains consciousness, keep them calm and in a recovery position. Opioid withdrawal symptoms may occur, which can be uncomfortable but are not life-threatening.
Handling Re-narcotization: Due to the short duration of naloxone, watch for signs of re-narcotization as the effect of the opioids may outlast that of naloxone. Have additional naloxone doses available and be ready to administer if symptoms of overdose return.
Use in Special Populations: In pregnant women, naloxone should be used if needed, as opioid withdrawal can be risky for the fetus. Adjust doses cautiously in elderly or patients with underlying health conditions.
Naloxone Limitations

Temporary Measure: It’s important to note that naloxone is a temporary treatment for overdose. Medical care is still needed as the effects can wear off before the opioids in the system.
Potency Concerns: In the context of extremely potent opioids like fentanyl, higher or multiple doses of naloxone may be necessary to be effective.
Ethical and Social Considerations:
- Stigma and Access: There’s an ongoing discussion about the accessibility of naloxone and the stigma surrounding its use, particularly in communities heavily impacted by opioid addiction.
- Empowerment and Responsibility: Making naloxone widely available empowers communities and individuals to act in life-threatening situations, but it also raises questions about responsibility and training for proper administration.
Naloxone Naming
Naloxone is known by various names and trademarks, reflecting its widespread use and manufacturing by different pharmaceutical companies. Here’s a list of alternative names and trademarks for Naloxone:
- Narcan: This is perhaps the most widely recognized brand name for naloxone. Narcan is commonly used in the context of emergency treatment for opioid overdose and is available in various forms, including nasal spray and injectable solutions.
- Evzio: This is another brand name for naloxone, known primarily for its auto-injector form. Evzio is designed for rapid and easy administration, making it user-friendly for individuals without medical training.
- Kloxxado: A relatively newer brand, Kloxxado offers naloxone in a nasal spray form, similar to Narcan, but with a higher concentration of the drug.
- Nyxoid: This is another nasal spray form of naloxone, available in some regions. Like Narcan and Kloxxado, Nyxoid is designed for ease of use in emergencies.
- Generic Naloxone: In addition to these brand names, naloxone is also available as a generic medication. Generic naloxone is typically less expensive and is available in various forms, including injectable solutions.
Each of these names or brands represents naloxone but may differ in terms of concentration, formulation, or mode of delivery. These variations are designed to increase accessibility and ease of use, especially in emergencies where rapid response is crucial. The development of different brands and forms of naloxone reflects the increasing recognition of its importance in responding to the opioid crisis.
Final Thought

Naloxone stands as a pivotal tool in modern medicine, particularly in the context of the ongoing opioid crisis. Its ability to rapidly reverse the life-threatening effects of opioid overdose has made it an essential component of emergency medical response and harm reduction strategies. The significance of naloxone in saving lives and mitigating the impact of opioid misuse and overdose cannot be overstated.
The importance of naloxone is twofold: Firstly, it serves as a critical emergency intervention, acting quickly to restore normal breathing in individuals experiencing an opioid overdose. This immediate action reduces the risk of fatal respiratory depression, providing a crucial window for medical intervention. Secondly, naloxone’s accessibility and ease of use have empowered not just healthcare professionals but also laypersons, including people who use opioids, their families, and community members, to act effectively in overdose situations.
However, the full potential of naloxone can only be realized through comprehensive education and training. This includes educating healthcare providers on the appropriate use and administration of naloxone, training community members and first responders in recognizing signs of opioid overdose and administering naloxone, and raising public awareness about the availability and role of naloxone in overdose prevention. Such education is vital in destigmatizing opioid use and overdose, encouraging prompt and effective response, and ultimately saving lives.
Sources for More
3. Pharmacists’ naloxone services beyond community pharmacy settings: A systematic review





Its so great seeing how much work you put into it. Thank you Alex!